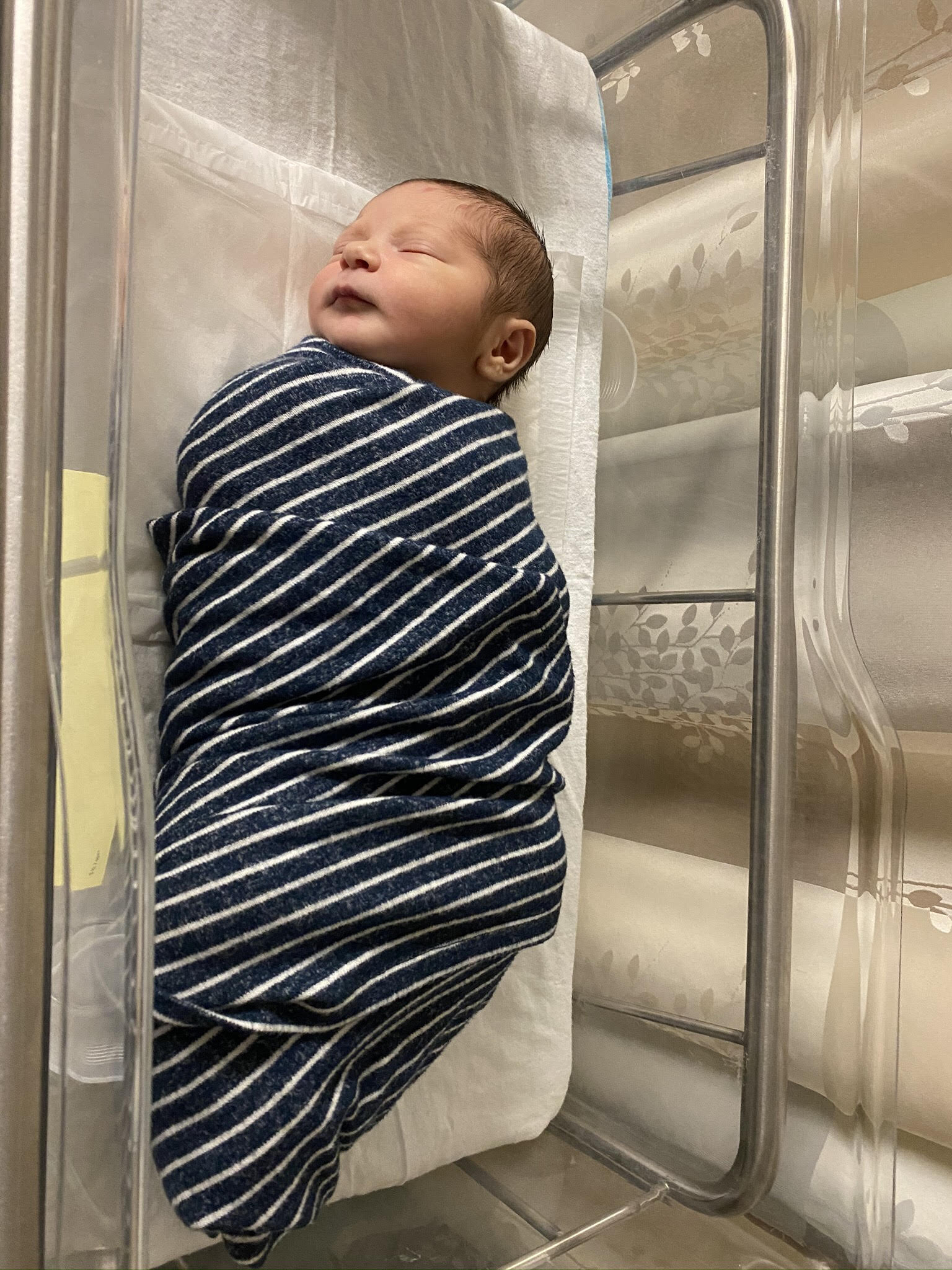
In the last couple of weeks of Jenn’s pregnancy and with the deadline set to induce labor, Jenn’s desperate to avoid induction and pulls out all the stops trying everything from bouncing on a yoga ball to red raspberry leaf tea because she had hoped for an unmedicated birth. Finally, sex seems to do the trick and her water breaks. When they show up to the hospital thinking they’d get to go home but instead get checked in, things play out in such a way that induction, epidural, and ultimately the assistance of a vacuum are needed for the over 24-hour labor. Also unexpected (and disappointing) twists were getting a different OB and different doula than planned. Jenn & Zach also share details about their fertility journey and about their son’s bris with a mohel.
Please note this story is one of the more challenging stories shared on this podcast, but it’s one that’s educational in ways that haven’t been shared thus far. Always check out the description here at the beginning of each episode or in the show notes over at birthmattersshow.com and decide for yourself which episodes you think will help you feel more confident and relaxed in the journey toward parenthood and leave the rest. Everyone’s preferences are different on this, so that’s why this podcast provides a fairly broad range of educational stories on this podcast.
Episode Topics:
Trying to get pregnant, having trouble after being on the pill due to having irregular cycles
Diagnosed with PCOS at fertility clinic
Started Letrozole but didn’t like the side effects
Stopped cardio exercise, eating more protein
Did more research and found Lisa Hendrickson-Jack - Get Pregnant Naturally program, game changer - read her book The Fifth Vital Sign
Went to see another fertility doc, no good
Switched to NYU fertility center - one round of Letrozole (pill) + trigger shot
Scheduled IUI, but timing didn’t work out due to the Thanksgiving
Conceived naturally on first try at that time
Trigger shot causes some confusion and false positives, some confusion over whether they were actually pregnant
Gender reveal party that got picked up by Sports Illustrated
Going to spend pregnancy living with Zach’s parents in the Hamptons, teaching preK remotely
Getting early pregnancy care out on Long Island
Hiring doula - should have interviewed together as a couple to find best fit for both of them
Moving into new apartment in Manhattan and shifting to NYC OB
38 weeks start talking about induction for 41w1d
Doula is sick for a couple of weeks, including when she goes into labor
Trying all the things to go into labor naturally - red raspberry leaf tea, spicy foods, bouncing on ball
Having sex seems to trigger spontaneous rupture of membranes early Friday morning plus bloody show, Jennifer is concerned something might be wrong
Her NYC doc was away on vacation; other doc on call
They arrive at hospital to triage and don’t allow her to go home
Calling doula, who’s still sick and recommends calling their sub, who she had just had one phone call with them previously
Doula arrives and debriefs - leads her in stretches and lunges
Took a shower; hydrotherapy really helpful
Used a TENS machine, helped with sense of control
Spent time on ball
Really hungry, eating Clif bars
Bought 1.5 hrs of time before inducing with pitocin
Couldn’t get off monitor to pee, had to use bedpan
Lots of vocalization
Feeling exhausted, not getting much of a break in between
Baby’s heart rate dips, they turn down pitocin, give her oxygen
Doc tells her she needs an epidural, Jenn feels like she doesn’t have an option and says yes.
Anesthesiologists were wonderful; they choose to have doula in room to support Jenn
Zach leaves the room and calls family, gets really emotional, Jenn doesn’t seem herself
He returns to room and Jenn is like a new person and it takes an emotional load off of him
Everyone taking naps, changing positions, doing cat/cow in bed
Directed pushing didn’t feel instinctive
Lots of people come in room, concerns about baby’s heart rate
Confusion over instructions
Asked for mirror in birth plan, didn’t get mirror
Zach had to hold her leg
Zach starts to see the head
Right around crowning and baby’s heart rate dips again
Attending comes in and starts giving instructions and tells Zach they’re going to use the vacuum
Vacuum pops off, which feels scary
Unpleasant experiences in postpartum unit, advocating for earlier discharge
Nuances and challenges of allowing family to spend time with baby in light of Covid, disagreeing a bit as a couple
Early breastfeeding - get help if needed
Circumcision/bris - didn’t have OB do it, hired a mohel/MD
Disagreement between Jen & Zach on whether to circumcise or not
Hebrew names after their grandfathers -- Avraham Simcha
Tricky diaper changes for the first 8 days or so post-circumcision
Tip from Jen - Go with your gut
Tip from Zach - Remember to advocate for yourself & be flexible and adjustable -- you’re not weak even if things need to change along the way
Resources:
Justisse International Fertility Awareness Education, Natural Birth Control & Reproductive Health
Jenn & Zach’s gender reveal tennis game party posted on Sports Illustrated
Dr Jeffrey Mazlin - mohel
Circumcision resource - podcast & written report (Evidence Based Birth)
Sponsor links:
*Disclosure: Links on this page to products are affiliate links; I will receive a small commission on any products you purchase at no additional cost to you.
Interview Transcript
59 - Jennifer & Zach Lerner - 2020-11-06 raw audio
Lisa: Welcome to the Birth Matters podcast. Today I have with me Jennifer and Zachary, or Zach -- you go by Zach, right? Yes. Welcome you guys. So good to have you on the show. Would you please just share with us how long ago you gave birth, maybe the borough that you live in, and if you'd like to share your professions, any of those kinds of basics?
[00:00:21] Jennifer: Sure. We gave birth, I gave birth on August 29, 2020 2:56 AM. And we live in lower Manhattan in Battery Park City, and I am a teacher, I'm taking this year off. [because of the] baby, but also because COVID has made things a little bit more complicated now with teaching and we thought it was the best choice for me to stay home.
[00:00:43]But I did do some remote teaching at the end of the last school year. And what age do you teach? Pre-K so three and four year olds, which is interesting over Zoom, for sure.
[00:00:54] Lisa: Wow. I cannot even fathom. Much admiration.
[00:00:58] Jennifer: It was tricky.
[00:01:00] Zach: And I am an attorney and I'm not taking the year off, unfortunately. So but I am working from home with COVID and everything going on. But it's working out, I get to spend more time with our baby, which is great. So I take a lot of "lunch breaks" in the middle of the day to play around with him and have fun with them. So it's very nice.
[00:01:20] Lisa: Nice. Thank you. Why don't you give us a little bit of background about getting pregnant and your pregnancy and preparing for this transition into parenthood.
[00:01:30] Jennifer: Sure. So we got married in 2018 and pretty soon after that we wanted to try to get pregnant. I was on the birth control pill for many years, probably like 12-ish years. Been on the pill since like college constantly. Sometimes changed the pill, but had been on it the whole time. And I had spoken with Zach about the fact that the birth control pill sometimes delay fertility and how I had issues with my cycles prior to going on the pill, which was the reason why the doctors recommended that I do go on it. Unbeknownst to me, the whole idea that the pill can shut down your body in terms of ovulation.
[00:02:11] And it can sometimes take a very long time for your periods and your cycles to come back. I didn't realize that when I was, you know, a college age person, a teenager, all of that. So I just thought, "Oh, if I go on the birth control pill, I'll get my period." Not knowing that it was like a breakthrough bleed and all of that.
[00:02:28] So since I learned a lot about that, but I had always had really irregular cycles sometimes when I was a young teen, I would have one period a year. At that time, I was just kind of like, "This is easy, great. I'm going to keep going like this." And you know, it was great to be on birth control pill.
[00:02:44] It helped my skin and some other things. I didn't really have any side effects, but I did know sort of later on that this could be a problem. And so in talking with Zach, I started with conversation of going off the pill because I thought that it could take a while for us to get pregnant if that's what we both wanted, which is what we did want.
[00:03:02]So I stopped taking the pill at the beginning of 2019. And didn't get a period for a while. I went to my OB I specifically went to find an OB instead of a GYN to assist me with getting pregnant and then eventually with my pregnancy. So I found somebody I really liked. I interviewed a couple of doctors.
[00:03:21] And after three months of being off the pill, I didn't get a period. So I went to go see her again and they thought maybe I had PCOS; they didn't really know. So they sent me to a fertility clinic which I did not like very much. I felt kind of like a number there. It just wasn't the best experience, but I did sort of start Letrozole cycle, which I then discontinued.
[00:03:44] I didn't like the medication; it made me feel kind of off. So I kinda just like stopped that experience then. And it was just really all about trying to naturally get pregnant. So from there I did a couple of recommendations that my doctor had suggested, like stopping a lot of like cardio exercise, not a big exerciser trying to eat more proteins and eat more overall.
[00:04:08] And I still, nothing happened for a while. A couple more months went by and I did more research and I found Lisa Hendrickson Jack, who is an awesome author. And she has a really great program, which is called the Get Pregnant Naturally program. So I decided to join it. It was an investment, but I really, I just thought it was so wonderful to learn about my body and also learn about fertility charting which was something I didn't really know anything about. How you can check your cycles naturally without taking a pill or getting an IUD or, you know when your fertile window is so that, you know, when you can have intercourse and so on and so forth.
[00:04:47] Lisa: And did you use an app for tracking?
[00:04:50] Jennifer: So Lisa suggests this particular, it's not an app yet. Maybe it will be one day, but it's more of like a website it's called the Justisse app. And Justisse, I think it's like a college where she got certified to be a fertility awareness educator. And I think it costs like a dollar a month or something like that.
[00:05:07] So I used that because that was really how she taught me to track my cycles. How to sort of note each day -- there's like a different color system and, you know, you check your cervical mucus, you check your cervical position and you check your temperature. So we learned all about that and super interesting. A lot of work, but it's great knowing that you're not putting, you know, chemicals in your body and having all these awful side effects that a lot of people experience.
[00:05:33] So I did her program. I learned all about it. I read her book. I made a lot of lifestyle changes in terms of my eating and my exercise and my sleeping and stuff like that. And after about six weeks of doing her program, I told Zach, I was like, "I just ovulated." And he was like, "No, you didn't."
[00:05:53] And I was like, "I'm going to get my period in 10 to 14 days," just watch. And I did. And I was so excited. I remember it was Father's Day. And I was like, and I wore this feminine dress. I felt like it was like my first period again. And it was very exciting. So after that I kept getting a period. I didn't get one the next month I got one the following month and the month after that, but then it kind of stopped.
[00:06:16] And we were sort of getting very impatient this whole time, you know, we had been trying, but we didn't realize that I wasn't ovulating. So we were kind of spent at this point. We made a decision to go see another fertility doctor that fertility doctor was also not good. So we decided to it didn't nix that one.
[00:06:35] And I finally went to NYU, which was wonderful. I really recommend NYU's fertility department. It was a great facility. The nurses were great. The doctors were great and it was actually a pleasant experience to go there. So for anybody that is seeking fertility assistance, I really recommend it.
[00:06:53]I did one round of a Letrozole cycle, so I started taking the Letrozole pill and I had to go in for monitoring every couple of days where they did an ultrasound and blood tests. And they would let me know if my follicles were growing, I had to purchase a trigger shot.
[00:07:09] But once my follicles were big enough, they would give me the trigger shot, which would induce ovulation. So, this was like last Thanksgiving. It was the Saturday of Thanksgiving that I came in and they said your follicles are 21 millimeters. And I was like follicles and they said I had two follicles.
[00:07:26] So I thought, you know, if I were to get pregnant that I would be having twins, but they said, do you have your trigger shot? I said, "Yes." So they shot me up with my trigger shot and they were like, "You can schedule an IUI for tomorrow." And we hadn't got insurance approval for that and it was Thanksgiving weekend.
[00:07:44] So it turned out that we couldn't actually do the IUI. So we were like, all right, let's just, you know, proceed. Let's just do it the old-fashioned way. And we actually got pregnant that first time which was incredible. I was already planning vacation around our next cycle because it was holiday time.
[00:08:03] And I wanted to make sure that I was there to be monitored and there was no way that I thought it would work the first time. But I really think a lot of the things that I did with Lisa had really prepped my body for pregnancy and I'm happy it worked out.
[00:08:17] Zach: One quick anecdote is that she was taking pregnancy tests kind of everyday after to see if she was pregnant and when you take this trigger shot, it induces a false positive on the pregnancy test because you have that hormone in your system. So we would look day after day and that line would get fainter and fainter, but then we get stronger and stronger again when you're actually pregnant.
[00:08:39] So it was a very difficult experience to actually figure out if she was pregnant with the pregnancy test, so we were studying them every day for like two weeks. And then we got pretty confident when the line got darker and darker again, that he actually was pregnant.
[00:08:52] Jennifer: It's called testing out the trigger shot, which is something that I learned in like some of these, like What to Expect groups, but a lot of women do it when they get the trigger shot and they see a positive sign and then it goes to nothing.
[00:09:03] And then if it comes back then you know you're pregnant. And of course I couldn't help myself, even though they say like, don't take a test until 14 days after your trigger shot. But of course I did it and we were like, I think we are, I think we are. And I started to feel some symptoms. I remember we were at a holiday party the night before I went to go take my blood test at NYU. And Zach was really, really positive that I was pregnant and he started telling all of his friends, I got really annoyed because I wasn't actually sure that I was. So then I went to the doctor the next day and we got the call sort of like midday and that we were, and we were actually going up to the Museum of Ice Cream that day and we had an appointment to be there. And we weren't sure like, you know, should we go, should we not go?
[00:09:49]We wanted to also surprise Zach's parents on the Upper West Side with special mugs that said, " only the best dads get promoted to Grandpa" / "only the best moms get promoted to Grandma". And we had preemptively got these mugs and we were like, do we take them with us? Do we not take them with us?
[00:10:05] We hadn't gotten the call yet. So we decided to take them with us and we're in the Uber. And we finally were around the corner from our apartment and we got the call that we were pregnant. And I was very cautiously optimistic because you know, it was very early and we were very excited and I know that my mom had a miscarriage early on after my brother was born before I was born.
[00:10:26] And I knew that this was something that could happen for sure. So I was just kind of like very subdued about it for a while. It took me a while to get excited. And you know, each time you go to the doctor, you're worried that you won't hear a heartbeat or you, you know, there's going to be some sort of problem.
[00:10:41] So I was very guarded in the beginning for a while, but as soon as we reached like the 14 week mark and I ended my first trimester, I sort of started to get very excited. We had a really fun gender reveal party the day after Valentine's day.
[00:10:57] Zach: We didn't burn down any forests.
[00:10:58] Lisa: Good, whew!
[00:11:01] Jennifer: [Our family?] loves tennis, so we did a gender reveal party with these plastic tennis balls that had colored powder inside. And there was, we had 10 balls to break. Four of them were the correct gender. Three of them were they incorrect gender. And three of them were yellow, which meant nothing. And so everybody hit a tennis ball and we've recorded it and actually Sports Illustrated
[00:11:21] Zach: Sports Illustrated picked it up and put it on their website.
[00:11:23] Lisa: No way, that's so fun.
[00:11:26] Jennifer: It was a lot of fun and it was a nice way to get our entire family together and involved. Not everybody always gets along, but this was a really fun day. So we were happy we were able to make it work. But yeah, after that, we kind of went right into quarantine a couple of weeks later, Zach and I went to live with his parents on Long Island from the mid-March to July, basically. And from there we were both working. I was finishing up my school year. My school was supposed to be on break. And then we found out that we were not going back to school, so we stayed out there. I was teaching remotely pre-K, which was tricky, but it was actually kind of happy for myself, selfishly, to be able to like, just be comfy at home because I was starting to get bigger and a little bit more uncomfortable.
[00:12:11] But it was great being away from the city to have some space, to not have to worry about everything that was going on. It was like the worst time. And actually we also had to move during that time, which added a wrinkle to our situation. But Zach went back and like packed up a bunch of our stuff and then we actually had movers move all of our things into storage and we delayed our lease until July. So it worked out. But it was a little tricky trying to figure out how we were going to do that. But it worked out, I received care in Long Island. I found a doctor's office out there, so I was going there pretty frequently that was during my second trimester, actually, not that frequently, but during my second trimester, that's when I was there.
[00:12:53] Yeah, it was just, it was fun. You know, spending time with Zach's family and being together, we got to go on walks a lot. We had the opportunity to play a lot of tennis, which was great. I got to sort of experience my pregnancy in a way that made me feel really strong and really happy.
[00:13:10] But you know, knowing what was going on in the city was also tricky, but I think it was a very healthy pregnancy. I ate well. I learned a lot in terms of like reading. I had a lot of time after the school year ended to read and read and read and educate myself about birth and taking care of babies and breastfeeding and all of that.
[00:13:27] We also took your course kind of during that time you know, early summer, which was so helpful
[00:13:33] Lisa: Virtually right?
[00:13:34] Jennifer: Virtually, we took it online.
[00:13:36] Zach: I would also say that.Jenn mentioned we played tennis and I know probably a lot of people out there are concerned to not take things too aggressively when they're pregnant and I'm not certainly not a doctor, so I'm not going to tell people what they should do.
[00:13:48] But Jenn was cracking the ball at me at 35 weeks pregnant. Now, maybe in hindsight, I shouldn't have run her around as much as I was running her around. But she was nimble out there and playing very well and looked like she was going to give birth any day. So it was fun.
[00:14:03] Lisa: That's great. I'm all for an active pregnancy. It makes a big difference in reducing aches and pains. And as long as you're listening to your body and not pushing too hard of course. But yeah, it's great.
[00:14:12] Jennifer: I definitely did not play to the extent that I previously played when I was not pregnant, but it was just nice to be able to move. And I do think it really helped.
[00:14:23] And I'll talk about that later, but as a big exerciser, I do think like it was really helpful in the labor process and, you know, leading up to birth and labor and also postpartum, I think it was really great to keep moving. So yeah, that kind of brings us back to New York City. We moved in July into our new apartment, which was a two bedroom to have a room for the baby. It was really tricky to move. That was really, it was really hot. And I was, you know, 33, 34 weeks pregnant when we came back. So my feet were swelling and I was just dying to unpack this whole apartment, but I really had to take a slow listening to my body. And then we started just going to the doctor, you know, weekly. We had our weekly checkups where we would do the stress then on stress tests.
[00:15:08] Zach: Before we get to this stage, Lisa, let me open it up to you. Are there any questions you have of us through this process up until now?
[00:15:14] Lisa: I don't think so. The one thing that comes to mind is at what point did you decide to hire a doula? And when did that come on your radar and you know, how did you choose the person, all that?
[00:15:24] Jennifer: So I'd say, I think it was around may and sort of like towards the end of my school year, where I started thinking about having a doula, which I wasn't sure whether doulas were going to be allowed. I think as soon as they found out that doulas were allowed in hospitals, I jumped on that opportunity.
[00:15:38] And after speaking with you about it specifically knowing in our conversations that I wanted to have a natural childbirth you suggested that I really look into the doula thing and I read the Birth Partner by Penny Simkin, which is an excellent book and learned a lot about birth partners and supporting somebody who's giving birth. And I felt like having a doula, especially during this time would be really helpful, especially for our first birth. And when I found out that doulas were allowed, I researched a couple of different I guess they're like agencies and had a couple of different Zoom calls with a couple of different people.
[00:16:12] And after doing like three or four different Zoom calls, I found somebody that I really liked. And unfortunately, Zach didn't do the calls with me. And I think when we had our intake call with our doula Zach was not too thrilled with her. So I would recommend if you, people are interested in hiring a doula for both people, both parents to interview the doula because it's important that they both--
[00:16:36] Zach: Well, I would also this: obviously, I think it's more important that the woman giving birth connects with the doula. We're different in some ways. For me, I don't know what giving birth is like, of course, but I think I would want someone that's more kind of a tender, loving person.
[00:16:54] Jennifer: Like you, Lisa. We should have hired Lisa.
[00:16:59] Zach: We really should have for many reasons. But Jen, I think sometimes responds better to someone who's more tough love kind of person. Like, you know, no BS kind of right in your face kind of thing. So in that sense, the doula we originally were going with exuded the latter. And I don't certainly judge Jenn for picking that. I think that's, you know, whatever she's going to respond to best is what she should go with. I think it was important for us, however, during this time to have someone there in person. I know a lot of doulas are offering virtual services during times of COVID that would've probably required me to hold up either an iPad or a phone a lot, or at least place it somewhere.
[00:17:40] Jennifer: I needed you to hold me up. Wouldn't work out.
[00:17:44] Zach: Obviously, despite taking your courses and learning stuff, you know, the doula is going to be better at the techniques and the massages and whatnot, than I'm going to be, so that was kind of something we required. And I would say for people that are looking to hire doulas, you know, to talk about the contingency if Covid does get worse.
[00:18:02] If it is very important to you to have someone there, we worked out something in our contract where if they were not allowed to be there, it was, you know, some sort of reduction in the rate of it's going to be virtual only because that was very important to us.
[00:18:17] Jennifer: Yeah. And we made that clear to our doula from the get-go that we really wanted in-person support. And I know a lot of people have talked about virtual support in terms of like, a lactation consultant virtually, or a doula virtually during a birth. But I really like appreciated what we learned about the different laboring positions. And I just like, I need that. I really want that. Especially during a natural childbirth, I want somebody doing massage to me or holding me or letting me do all the different positions.
[00:18:44] So we had found that doula and we had our prenatal appointment in July and we went over my birth plan, which I had made for many months revising and working on.
[00:18:57] Lisa: With your doula were those virtual prenatals or--
[00:19:01] Jennifer: That was virtual as well, yeah. So we had our doula and then moving on from there. We're now back in the city, we had weekly appointments. So we're going to our doctor's office. You know, it was very stressful with getting into Ubers and, you know, cleaning everything and making sure that everybody was safe.
[00:19:16] But we had our appointments and then towards like 38 weeks or so they started talking about induction and you know, what that would be like, they explained to me and Zach that they didn't want me going past 41 weeks and one day. And to this, I was really upset because I had explained to my doctor that I wanted a natural childbirth and I did not want to be induced.
[00:19:40] And I understand in terms of COVID, when COVID was really bad, maybe I would be interested in an induction because you want to be sure when you're going to be in hospital and, you know, be there for the least amount of time, but COVID had gotten a lot better. And so I really just wanted to go into labor naturally.
[00:19:56] That was really important to me. So I was starting to sweat a little bit by 38 weeks. And actually I did think that it was possible that I was going into labor at 38 weeks. Cause I was kind of like having like a little bit of leaking and I wasn't sure if it was amniotic fluid, I did call the doula and just to check in with her.
[00:20:14] And she was like, Oh, you know, if you do go into labor tonight, just know that I'm sick, so I can't help you. I have to have my sub help you. And I was like, okay, I didn't think that it was really me going into labor, but I was like, great, well, she's sick now. She's going to be available, you know, in 40-ish weeks when I do eventually give birth.
[00:20:34] So it turned out, you know, I was fine. I was fine then. And nothing happened. We just kinda went on and I was working on bouncing on the ball and doing all the things to sort of try to bring on labor. And then we went to our, was it like 40 weeks, I guess? And they were basically like, we had a lot of back and forth about the induction process and we're getting sort of late into the pregnancy.
[00:21:01] And they were basically like, we're scheduling your induction. And I was really upset about this and we sort of went back and forth about whether we would try to like, get a different doctor last minute or a different hospital. But you know, we kind of like stuck it out with this doctor. And we wanted to do anything we could to sort of induce labor naturally.
[00:21:20] So by like that 40-week mark, where I'm having spicy food and I'm drinking red raspberry leaf tea, and I'm eating dates every day. And I was setting up an acupuncture appointment with somebody that you recommended to me. And then at one point, Zach looks over at me and he's like, "Why don't we just have sex?" Like we could, we could possibly induce labor naturally, and we won't have to, you know, deal with the timeline of the doctor and it's free.
[00:21:46] So that's great. So we decided to do that and, you know, it was interesting being 40 plus weeks pregnant.
[00:21:54] Zach: And literally five minutes after her water breaks.
[00:21:59] Jennifer: I wasn't sure that it was my water, but I was sort of like, it was, it was, I guess this was Friday morning very early and I hadn't gone to sleep or anything like that. And I felt this pop and I actually heard it and I felt it at the same time. And it was something like I've never felt before. So I was just kind of like Zach, I think my water broke. And he was like, no, that didn't happen. And I was sort of leaking something. We weren't sure what it was. It could have been something else, but we just like were really unsure about it.
[00:22:30] Zach: Does your podcast have like a rating? PG-13? We can censor this part.
[00:22:37] Lisa: It only asks about profanity, not the other thing.
[00:22:39] Jennifer: I was really not sure what was going on, but I had also experienced some blood and it was like, it came to be quite a lot of blood, which really worried us. And we decided we were going to call the doctor and see, I knew about the bloody show and the mucus plug.
[00:22:55] And I had been educated about all that, but it just seemed like a little bit different to me. And in that moment, I was panicking a little, like, what if we hurt the baby? What if something went wrong? Not that I think having intercourse when you're pregnant would hurt the baby, but like something else, it seemed like could have gone wrong.
[00:23:11] So I have these two things happening and all of our bags are packed and I'm like, I don't know what to do. So we called the doctor that was on call and it was actually the doctor that I spoke to was the doctor that delivered me was not my doctor. I hadn't mentioned that my doctor was away on vacation. My New York doctor.
[00:23:27]And so she was like, "I don't really know, but you should come in." And I was like, "Should we bring all of our stuff?" And she was like, "Yeah, bring everything." So we're like, okay, Zach didn't want to bring the car seat because we thought we'd be turning around and coming right back home. But we brought everything.
[00:23:42]We probably left our apartment at like 2:00 AM or something like that. And our Uber ride was pretty quick. Nobody was on the road, you know, it was COVID but also in the middle of the night. So we got to the hospital, we had our temperature taken and we went right upstairs to check in. They took me into triage and I thought that they were going to check me really quick and like, you know, I was going to be admitted or not, but that was foolish of me.
[00:24:04] Something else that I should have thought about. I didn't even take my phone with me. I literally just took my body and I left Zach with all of our stuff and like the little check-in area. So they took me in and I was waiting for hours and hours. Nobody was there but I was still waiting for hours and hours for the nurse to hook me up to the machine to get changed.
[00:24:23]My doctor finally came in. And she was like, "All right, I'm going to check you and we'll see if this is like, what this leaking is." And so she, some sort of like stick, she stuck up there, pH test. The pH test. And she said, if it turns blue, it's amniotic fluid. So it turned blue. Sure enough. And so I'm like, "Oh, no. My water did break and I'm at the hospital."
[00:24:50] My original plan was to stay at home for hours and hours, but now I'm on their time schedule and I'm on the clock for sure. And so I was really disappointed at this point. I was also not with Zach and I couldn't text him. So I was alone. Kind of upset, but also really excited because I knew my baby was coming soon.
[00:25:07] Zach: This became real for me when I joined her back there and there was a nurse and I said to the nurse, "Well, like, do you want us to go home? Because you know, we came in so quickly?" And she goes, no, when you leave the hospital, you're leaving with a baby. And that was the moment where I was like, ah, this, this is real. This is happening. Yeah.
[00:25:24] Lisa: And that's something I feel like I need to make more clear in class is that with the vast majority of care providers, if you go in and they confirm your water has broken, it's going to be almost impossible to leave. There's a midwifery practice that works in a hospital here in the city who a client worked with.
[00:25:42] And they are the only practice who I know of who advocates for the person to be able to go home. If it's a low risk, healthy pregnancy, there's no risk factors that they can see, you know. But it took some even advocating on the part of the midwives to convince the attending and the nurses there to let them go.
[00:26:07] So it can be challenging and it can be surprising. And a lot of people will show up, like, just like you did thinking they're going to go home and it's good you brought your stuff because many people show up and they didn't bring their things because they were totally sure they were going home.
[00:26:20] Jennifer: Yeah. I had like all the stuff on your Amazon list.
[00:26:26] Lisa: You're one of my most prepared students, reading all the things,
[00:26:30] Jennifer: I was prepared. All the foods, all the drinks, the Miso soup, the coconut water.
[00:26:34] Zach: You know, I, I do want to say that it's great to be prepared and I'm glad we were, but it's almost like the, I think it's going to draw analogy to boxing. Mike Tyson once said everybody has a plan until they get punched in the face. And when you start actually going through this, like Jennifer had everything ready.
[00:26:52] Jennifer: I had read like 15 books.
[00:26:54] Zach: Then when you get to the actual labor, things could get turned upside down really quickly. So I guess if I not to jump too far ahead, but if I were to give a recommendation to people listening, be prepared, but don't get overwhelmed if you need to call an [audible?] or change things in the middle. I think, you know, from seeing what's happening around us and then watching Jenn as well and hearing screams and other rooms, I think it's natural to realize things are going to get rocky, but, you know, as long as you're prepared for it mentally as well, you can get through it. But it's easy for me to say, I'm just standing there saying, yeah, Jen, you're doing great.
[00:27:30] Jennifer: So that's a really good analogy. So finally Zach was able to join me in the triage room after they confirmed that I was admitted and I wasn't going anywhere and they weren't gonna let me go. So we started like calling parents and stuff like that.
[00:27:44]And somebody was like, "You should call your doula," because I gave them my birth plan. I was like, "Oh yeah, I should call my doula." I was just so out of it. And so exhausted at this point. We call the doula and the doula said, "I'm still sick." And I was like, what? I was like, I thought you were sick two weeks ago; you're not better? And we had been communicating during that last two weeks of my pregnancy, or is it more like three weeks? Because I went into labor at 40 weeks, five days. And we had been communicating about different things that were happening. My prenatal appointments, things like that. I was like, why didn't she mention that she was still sick? I was expecting her to join me. When, you know, the time came
[00:28:21] Zach: And as we indicated earlier, it was very important to have someone there in person. So we would have hoped she would have been communicating about the potential that she couldn't be there because of whatever illness she was going through.
[00:28:33] Jennifer: And that was not communicated at all to us. So she said to me, well I can join you virtually, or I can send my sub. So I said, "Well, let's do the sub." Because like I said, previously, like it was in our contract. We really want the in-person support. That's really important to us, you know, it's going to be very hands-on. You know, I wanted it to be as natural as possible.
[00:28:53] And so she said, "Okay." And actually at the 38-week mark had called the sub doula. So I had spoken with her before, when, you know, I thought maybe that night I'd be going into labor. Just, I was going to ask if you had met her. Yeah. So I hadn't met her like over Zoom call; it was just a phone call. So I hadn't seen her or anything like that.
[00:29:11] It wasn't really like a meeting. The sub doula I called and she said that it would take her about an hour to get to where I was. And she said, "What would you like me to do?" And I was like, "I'd like for you to come right now." You know, I didn't have my doula, I didn't have my doctor. You know, we are on the clock. I'm like, "You should come." And then we had our COVID test in triage, and then they moved us to the labor and delivery room.
[00:29:35] Zach: I don't want to move off of the doula point yet because this may be interesting to you as well and said, you know, maybe, I don't know a lot about the doula market in general, you obviously do, but Jenn did a fair amount of research. She wanted someone very specific with you know, specific experience number of years. I think the person we chose had special training and certain techniques as well. Yeah.
[00:30:00] Jennifer: Yep, Hypnobirthing. And she was actually a personal trainer. And so I was like, she's going to be very strong and capable of like helping me with all the physical stuff.
[00:30:08] Zach: So as a result, I think it's fair to say we were paying a premium for her experience and expertise which I completely understand she has this expertise. She should charge more. And I guess it becomes difficult because life happens. I'm sure with you as well. And other doulas, if something happens, you can't be there, you arrange for a sub. But if the sub doesn't have the same qualifications as the person you picked or the experience. Again, that happens, we have to do the best we can, but there was no mention of any sort of negotiated discount if you had to use a sub or anything like that.
[00:30:42] Jennifer: Right. We hadn't foreseen that being an issue and we probably should have.
[00:30:45] Zach: And I think in our view, and we could talk more about the actual birth. I'm not saying our sub was deficient or anything. But if we had wanted someone with the experience and training of our sub, I think it would have been about half of what we were originally spending. So that was a real issue that comes up. And I don't know how to the doula market in general deals with these contingencies, but it was something that did bother us.
[00:31:10] Lisa: That makes sense. And one thing that I would just point out for these weird times we're living in with COVID. Backup relationships have been trickier because there's so many doulas when you were giving birth were still only attending virtually. And so the options for a backup, might've been a lot more limited. So that maybe in normal times, their backup would have had the same qualifications or very similar anyway. So I suspect that might have been a factor. I don't really know, obviously, but that's just something that comes to mind knowing what I know about what's going on in the doula community, that that's been so tricky to find in-person backup.
[00:31:47]But I'm sorry that that happened to you. And I think that's going to be helpful for listeners to just come up with the questions that they want to ask when they're interviewing doulas. So thank you for that.
[00:31:56] Jennifer: Absolutely, yeah. To make sure that you get to meet that doula over Zoom. I remember my first doula, the doula that I hired said something about, you know, forming the relationship with the sub doula, but it was actually never a part of our prenatal appointment.
[00:32:12] And there was so much that I wanted to ask her that I didn't really get to that, but I think that was being optimistic thinking I'm going to have this one. But I say to people, don't be optimistic and definitely think about that stuff, even though it's not something that you do want to be thinking about, but it's something that you want to have thought about if it does happen.
[00:32:28] Lisa: Yeah. And a lot of doulas are working on a partnership basis rather than like a backup kind of basis where they do as a pair, they'll do the prenatals together. So you've equally gotten to know both of them. Yeah. So that's another model that somebody could seek out if they would prefer that over the sub where you're much less likely to get to know the sub.
[00:32:49] Jennifer: Yeah, like a team. I like that. That would definitely be something that I consider doing this again, looking for another doula for a future pregnancy. So we called our sub doula; our sub doula's coming. Zach was really mad that our original doula was not there. And of course I'm dealing with, you know, my water having broken, being in the hospital way too early, no doula, no doctor and I was just trying to stay positive.
[00:33:15] I was like, relax. I know, like this sucks, but we're, we're gonna have to just keep going. And we did and went into the labor and delivery room. We got all of our stuff set up. I was having contractions, but I wasn't really feeling anything and is like, I'm really tough. You know, this be fine. I'm doing great.
[00:33:35]I barely felt anything. And from then our doula came and we sort of filled her in on what was happening. She wanted to then start helping me and she led me in like some stretches and some lunges and stuff like that. We were just talking, trying to get to know each other. Everything was pretty easy at that point. And I don't know how many hours were was I laboring naturally, do you remember?
[00:33:58] Zach: I'm not sure, it was a number of hours, but it progressed exponentially when it started. You know, Jenn was doing different exercises on the exercise ball and then, you know, our backup doula was helping her and giving her some massages.
[00:34:12] Jennifer: Yeah, I would have liked some more massaging.
[00:34:14] Zach: Yeah. You know, we learned a lot in your class and she obviously knew the techniques. I was hoping she would do the massage through every contraction, but she, it was kind of sporadic.
[00:34:23] Jennifer: Yes, she wasn't. I definitely, I mean, I know it takes a lot of muscle and strength, but I definitely thought I would get a little bit more of that. I took a shower, which I was really happy I did then. The bathroom was awful, but it was really great to labor in the shower, which is something that I had learned in your class, but also something that I thought like I would really enjoy--being in the bathroom and taking a shower. And she gave me a TENS machine, which we hooked up and I was using that, which I didn't really know that much about.
[00:34:54]But I was happy that she had it. It was a small little thing which would sort of give me like a little like sensation when I pressed a button. And I would do that, I would press that button for as long as the contraction lasted. And then when I pressed it again, it would stop. And the doula explained that this would give me some sort of sense of control over the contractions.
[00:35:13]I don't know how much it helped me, but I think the sense of control was really great, especially considering my situation. So I used that. I spend a lot of time on the ball, rolling around and bouncing and doing different techniques that we had learned and that the sub doula was leading me in, we went on like that for a while.
[00:35:31]I was starving. I was really hungry because I hadn't eaten since the previous night -- dinner at like, I don't know, eight o'clock. So hadn't slept, hadn't eaten. Trying to labor naturally. And eventually the doctors and nurses were sort of coming in and they were kind of like looking at the clock and they did check me and I had only dilated about a centimeter.
[00:35:51] Lisa: Do you have any sense of when this was? What time did your water break-ish and then when was this?
[00:35:55] Jennifer: My water broke Friday morning at 1:00 AM. We went to the hospital at like a little after two. So we had to like gather all our things and get there. We went into labor and delivery probably around four and then I'm laboring naturally. I don't know--
[00:36:10] Zach: A couple of hours, maybe three, four hours.
[00:36:13] Jennifer: I thought it was more than that.
[00:36:15] Zach: It may have felt like more than that.
[00:36:16] Jennifer: Oh, well, yeah, sure. I don't know. Maybe four to six hours would be like a rough estimate. Yeah, obviously the timing sort of,
[00:36:24] Zach: But she wasn't dilating and they wanted to start the Pitocin to expedite the process.
[00:36:31] Jennifer: And we were all like no, no, no we don't want to
[00:36:34] Lisa: That's so quick. Whether it was two or three or four or six, anything in that range is very soon to be saying you're not progressing.
[00:36:43] Jennifer: So we really worked hard to push them off as long as we could. And we got about an hour and a half of time sort of alone, where they weren't really bothering us unless we needed something, of course, and the nurse would someone bring it. But it didn't seem like a lot of time. I would've liked to have more time, but they came in and they were like, okay, it's time for your Pitocin. And I think the worst part of the Pitocin for me was that I had to be hooked up. I didn't have to be in bed, and I could be on the ball, but I had to sort of be near the bed.
[00:37:12] Zach: And I think, one of the, you know I don't know if it's really talked about a lot, one of the disadvantages of being hooked up, not only can't you do as many of the exercises maybe you want to do, but the privacy rights. You had to go to the bathroom, she couldn't even get to the bathroom, you have to have a bedpan.
[00:37:28] Jennifer: It was awful. I think I started to cry and I couldn't
[00:37:32] Lisa: So dehumanizing, right?
[00:37:34] Jennifer: It was so bad. And I had to go and I was just like, "I can't go with you two in the room." And like all these people in and out, like it was awful. So yeah, I struggled with that a lot. You know, not having the freedom, but also not having privacy. It was very dehumanizing.
[00:37:51] Lisa: Just to clarify for listeners, I assume the reason you were restricted in your movement was because of continuous monitoring is necessary with Pitocin. Yeah?
[00:38:00] Jennifer: Yeah. I had to be hooked up--
[00:38:01] Zach: And they didn't have the Bluetooth monitoring.
[00:38:03] Jennifer: Of course, yeah, I had asked about it, I knew that in advance. I did know that they did not have the wireless monitoring. I knew at some hospitals they do, but at this particular one they did not. And yes, I did know that once I was on the Pitocin I'd have to be hooked up. I did have a heplock previously. I did ask for that. I remember asking for that in advance when I give my birth plan and they were like, "We'll hook you up." And I was like, "heplock?" And they were like, "Okay." And that's when everything was, you know, very peachy. But at this point I kept going with Pitocin, just kept trying to do as much as I could, with different positions and laboring on the ball. I was doing a lot of moaning and screaming and groaning. I used the TENS machine.
[00:38:42] Zach: This is where the labor things picked up. And I think it's important to remember, you know, we had been up the whole previous day, normal day and her water breaks at 1:00 AM. So now we haven't slept at all through the night. Now you're getting to, you know, normal like wake up time, right? The late morning, we're all sleeping deprived and she's now having horrible pain. So she's having these mini naps, you know, for 30 seconds to a minute between contractions and getting woken up and in terrible pain.
[00:39:11] Lisa: Yeah, because Pitocin usually brings those contractions, make them stronger and harder and closer together, which can be very hard to tolerate, especially when you're exhausted.
[00:39:20] Jennifer: Absolutely. I remember leaning over, I was sitting on the ball and leaning over onto the bed and just sort of like had my head on my arms and I would take these little naps sort of in between. It was just like really needed them. And yes, it was quite a startle when I woke up from a contraction. It was, it was tough.
[00:39:38] It was definitely, it was getting really hard and something that I remember, which I know we've spoke we spoke about in class was that the monitor will tell you when the contraction supposedly starts and ends. And then I remembered the doula and Zach and be like, "It's over." And I'd be like, "No, I still feel it, like stop saying it's over."
[00:39:55] And I started getting really snappy at them for that. I just, you know, it was hard thinking, you know, they think it's over, but it's really not. So that was another like little sticking point that was irritating to me. So we kept going, we kept going and going and going there wasn't really much that I could do, you know, in terms of exercises, I tried as much as I could.
[00:40:15]And then the doctor came in and she was like, okay, you have to get an epidural. And I was like, "I don't want an epidural." And she said to me, well, if you have to have a C-section, you're not going to be able to see your baby.
[00:40:29] Zach: I'm sorry to interrupt Jenn. But we skipped over kind of the impetus for that, which is the doctors came in and the heart rate was dropping for the baby. Yeah. And then they put Jenn on supplemental oxygen. They did cut the Pitocin and a bit to try to help restore the heart rate and they threw quickly oxygen onto Jen's face. And then the doctor kind of quickly leaves and I go out of the room to find a doctor.
[00:40:59] And I said, "Is everything okay? Like, you know, people just rushed in here for the heart rate dropping and you just threw oxygen on Jenn." And he basically told me, "Yeah, things are fine. You know, we just have to be prepared for, you know, emergency C-section." And that was kind of the impetus for saying to Jenn that you need an epidural or else you won't be able to see your baby born. If you have to go to for a c-section.
[00:41:23] Jennifer: It was so upsetting, you know. The way that she said it, she had like very little bedside manner. And she was like, well, if this happens and I was like, what? Like C-section? Like, who said anything about a C-section? And like, why is she saying it like that to me. I didn't know that conversation, or at least didn't remember until now that that happened.
[00:41:42]But yeah, at this point I was just so exhausted and upset and crying again that like this had to be the next course of action. And I just, I couldn't like, I, it was really hard for me to go on. So I guess in hindsight, it was better to have the epidural, even though I didn't want it, but based on everything that had happened in our journey up to this point, it was probably the right decision.
[00:42:05]But obviously not the way that I wanted to give birth. I wanted to be a little bit more in tune with my lower half. But so from then the anesthesiologist sort of like appeared. It was like all of a sudden, because it's so foggy for me. And they were probably like the nicest people that I had encountered in the hospital.
[00:42:24]They were amazing and I was so nasty to them because I did not want this epidural. And they were like, so you want an epidural? And I was like, "They're making me get an epidural, I don't want one." So they're like, okay. And they just happily like went on with their little explanation of like what it will do and how it works.
[00:42:41] And you know, where the needle will go. And I was like, "I know all this, Lisa taught me all this," but... So they did say that I could only have one support person in the room when I was having it inserted, which I think we also talked about. So we actually had Zach leave and we kept the doula in the room with us because we thought that she might be able to position me in the right way that I needed to be positioned.
[00:43:03] And Zach had never, you know, supported somebody getting an epidural before. So he went out into, I guess the waiting, I didn't even know you could leave the room, but apparently you left the room.
[00:43:12] Zach: I'll take it from here on this part. I leave the room and I go out to the waiting room and I took this as an opportunity to call our family members to tell them what was going on. And I started breaking down a bit because you know, the risk of emergency C-section the heart rate dropping Jenn basically was a zombie. Like she couldn't form sentences. And I'm talking to them, breaking down a bit, you know, they're saying, hang in there, things are going to be okay. And then I returned to the room, about you know, I guess, 20 minutes later.
[00:43:41] So Jen's having just full blown conversation with the doula. Like, you know, she's just chatting at a cafe and there's no COVID in the world. And I couldn't believe what I had seen was complete night and day. And I guess what I would say in general to talk more about her experience is that. I completely respect Jen's right and every woman's right to do the birth, however they choose. I made a promise to Jenn that I would never say to her, you need to do this. You should do this. And just kind of you know, be there for her during this. But you know, I gained more life watching her respond so well to this and she pretty much from there on out until the very end -- we'll get to the pushing process -- was a very enjoyable experience, I think watching, she got, you know, real naps now and was able to just kind of breeze through the process a bit. I understand many people don't respond quite as well; Jenn did. You never really know, but I am so glad given what she was going through to see that pain taken away from her, seeing her go through that pain was killing me.
[00:44:45] Lisa: Thank you Zach, for sharing that. I'm so grateful you shared that. First of all, we just need to hear more of the partner's perspective. I love that you said, I believe you phrased it as, "I gained life coming back into the room and seeing her just seem more normal and not be in such pain." So it's so important to realize like there's a whole emotional arc to this journey for partners as well. Yeah. And it can be so hard to see your beloved in this kind of discomfort or pain that, that you've never seen them in before. Yeah. So thank you for sharing that.
[00:45:20] Jennifer: And that was one reason why I thought it'd be really helpful to have a doula, especially for our first birth, because it is hard to see your beloved and in such pain, but it is normal to be going through all of this stuff. So to have somebody to be like, yeah, this is what happens. And you know, that is also helpful for people that are coming up, you know, a first or even a second birth.
[00:45:43] Zach: But you know, I will say that on top of going through the normal pain that most people go through during childbirth. You also need to remember the timing was just so horrible for us now, Jen, hadn't slept for a day and a half. If somebody's incredibly sleep deprived going through this, it just compounds the magnitude of the disarray going on.
[00:46:04] Lisa: Sure. And you might not have had the energy to push the baby out and give birth if you hadn't been able to get some rest, it totally makes sense. We're glad we have this as a tool when it's needed.
[00:46:14] Jennifer: Definitely. So from then on, we all kind of like took naps after I had the epidural, I was just like, "Wow, I can see why people do this. This is different, definitely different. It felt so much easier."
[00:46:27]And we kept on sort of going like that for a while. They checked me, I think at six centimeters. And then again at like eight and a half, nine centimeters. And they sort of let me know that I would be starting to push. And that was sort of when we heard screams from other rooms. And I remember my doctor having the door and be like, "That won't be you." And I was like, "Okay, well I think it probably will be."
[00:46:50] Zach: Obviously we had spoken about this in your class. You see a lot in the movies and TV shows --someone goes into labor in the next scene, you know, 15 minutes later they're supposed to give birth. So of course we all know at this point, that's not true, that's not what labor really is like. I thought maybe the converse is also true that, that horrible screaming you hear in movies, maybe that's not true. I was wrong. The screams I was hearing from other rooms -- and we'll get to Jenn in a moment -- [maxed] what you see in movies, or at least that was my experience. I don't think I could scream that loud without tearing my vocal cords.
[00:47:25] Lisa: Jen, could you just speak to a little bit of something you wrote about in your written version of your story? When you were laboring in the bed and resting and everything, I think you mentioned that your doula got out a peanut ball and that you were changing positions regularly.
[00:47:38] Jennifer: So she brought a peanut ball with her and she kind of like tucked me in and we would sort of alternate like every 30 to 45 minutes, the different sides. And that was really, I think pretty much the only different position that I could be in when I was in bed now with the epidural. And also had a catheter obviously. But towards the very end of my time before pushing, we asked the nurse, if we could sort of position me in like a cat-cow position so that I could do that for a little bit before the pushing to sort of try to get the baby a little further down. And so I did that probably for an hour or so before the pushing began, which I hope helped, I don't really know,
[00:48:17] Lisa: So you had some feeling in your legs in order to do that?
[00:48:20] Jennifer: I think I did. Yeah. And it was also then like intermittently, like taking naps again you know, on my arms, you know, trying to rest that I could to like regain strength and energy for like the big event that's coming too.
[00:48:34] Lisa: And did that take like special advocating for yourself? For the nurse to allow all fours?
[00:48:40] Jennifer: Yes. The doula had actually really pushed and this was like the first time that she was like pretty vocal. I hoped that she'd be a little bit more vocal earlier, but she was really into me trying to, to get into these different positions towards the end.
[00:48:54] And she, I think, thought it would help and be beneficial to me. And the nurse was kind of like thinking about it. I could tell that she didn't really want to, or didn't think that it was okay, but she did like move the IV and stuff to position it so that we could do that. So that was really great.
[00:49:10]So we did that for a while. And then they came in and they told me, you know, now it's going to be time for your pushing. And they taught me how to breathe and push during that time. And it felt really uncomfortable to me the way that they taught me. You know, you have to like, hold your breath.
[00:49:25] And I felt pretty uncomfortable doing it that way. But at this point, there's nothing else that I could do; I didn't know an alternative. And there were a bunch of people in there that were telling me what I had to do. And they were being very pushy and very bossy. A lot of people came in at this point.
[00:49:40] I had the oxygen mask on all of a sudden there's like 10 people in the room. I guess they were starting to get very concerned about the baby and heart rate dropping starting to get very stressful. I was trying to adjust to like the breathing and pushing, practicing that and
[00:49:55] Lisa: And were you feeling pretty numb at this point? And were you able to feel the urge to push at all?
[00:50:00] Jennifer: I hadn't ever pressed the epidural button to get more medicine because I intentionally wanted it to wear off a bit during this time.
[00:50:07] Zach: This is when the pain came pouring back.
[00:50:10] Jennifer: Well, the pain was like the pushing. But I don't remember feeling like as much pain as I did earlier. Like with Pitocin or when laboring naturally. Like I felt contractions, but I didn't feel it anywhere near as tough as I did earlier, but the pushing was definitely painful. But yeah, a lot of people were in the room. It started getting like a little chaotic. I was like, so out of it, and then like trying to prepare myself to push out a baby, everybody's telling me different things when the pushing started and we were doing sort of like sets of three. And I had asked for a mirror, I didn't get a mirror and I had no idea like how far along I was. And I was kind of out of it. So maybe Zach wants to tell you...
[00:50:50] Zach: Yeah, I'll talk about it from the partner perspective at this lovely time in the process.
[00:50:55] Jennifer: I was not really there.
[00:50:56] Zach: I was positioned down by like her hip area.
[00:51:00] Jennifer: You chose to be there.
[00:51:02] Zach: I was helping folding her legs a bit. And I actually had ambitions of maybe taking pictures or recording it. As it turns out that was a silly ambition because [inaudible] in the room, they would have just been appalled if I took out a cell phone at this point.
[00:51:18] Jennifer: Would they have even allowed you?
[00:51:21] Lisa: They often don't allow video.
[00:51:22] Zach: I don't get kind of grossed out too easily, so I thought it'd be a cool little thing. I've kept some weird things from our boy since he's been born. But anyway, those are different stories.
[00:51:32] Jennifer: I know what you're talking about.
[00:51:33] Zach: So you know, we're helping her through the pushing process and she was describing the, you know, pushing for 10 seconds kind of thing. And again, I started get a little worried again because she was now starting to get a little delirious again, and the pain was kind of pouring back with the pushing.
[00:51:49] And, you know, at the same time I'm watching the doctor during the contractions and during the pushing, help facilitate the pushing. And it was a, a learning experience for me. And, you know, I don't know how much we may have gone over this in class or the stuff I was reading, but it was surprising how much the doctor facilitates the pushing process as well, literally, you know, goes inside of her and does techniques with her fingers to, I guess, help pull the baby out during each pushing process. But you know, I obviously can't put myself in the situation, but it's a pretty aggressive movement she would use. So on top of Jenn pushing, I can't imagine what she was feeling to have, what I can only assume as much worse than traditional gynecologist giving you an examination.
[00:52:36] Jennifer: I don't even really remember that, like feeling that. I just remember like, feeling like an overall sense of pain. So I don't even think I realized that was happening. And Zach explained it to me later and I was like, oh.
[00:52:48] Zach: Right. So then as the pushing is going on, you know, I start to see the baby's head a bit and she points out the baby's head.
[00:52:55] Jennifer: I had no idea.
[00:52:56] Zach: This is when it got really real for me. Cause I could see some little brown hair, you know, on top of his head. I was like, "Oh, well that's interesting 'cause Jen's kind of blonde." So now we know what his hair looks like. But that is, you know, a cool first experience with the baby, you know?
[00:53:09] Jennifer: I really wanted to mirror cause I had no idea. They kept saying like, "You're doing great. You're doing great." And I was just like, thinking, "I'm so tired." And like, I'm a strong person, but I knew I wasn't like up to my full potential after all of this and had no idea how far along I was.
[00:53:24] Zach: Then another scary moment here is that she's pushing. But I guess the baby's heart rate starts going down during the contractions and the pushing. And people start rushing back in to the delivery room, including, you know a more elderly woman who must, must've been the head of the ward at the time, which makes you panic that they're calling and someone you haven't seen all night and there's, you know, seven different people in there. They're giving her oxygen again,
[00:53:49] Jennifer: She's giving orders to everybody, telling them what to do.
[00:53:52] Zach: So then we're getting closer and closer. And the doctor looks over to me and says, we're going to use some sort of suction cup, the vacuum to help get the baby out. Now at this point again, Jenn is back into delirious stage.
[00:54:06] So I'm thinking kind of what you discussed in our class, talking about the risks and everything like that. Unfortunately, you know, in a situation like Pitocin or whatnot, you have the time to talk about, "Oh, what are the risks and whatnot," but when the baby's starting to crown and you have an army of people around you, you know, waiting on your decision. So I say to her, what are the risks? And she
[00:54:29] Jennifer: I remember you, like, sort of like screamed it.
[00:54:34] Zach: Oh, you know, some lacerations on the head. And I was like, what does that mean? Does that mean a paper cut or does that mean you could, you know, cut the baby's head in half? I don't know. But I did consent at that point. I'm basically Jen's proxy. And like I said, there was an army of doctors, so I didn't want to make a call as the baby was being born that can harm the baby. So, so I consent. So they use that and the baby's coming it's coming. Then the head is, you know, nearly there. And then the vacuum goes flying off the head. Just pops off.
[00:55:08] And I look at our baby and I see like a big ring around the baby's head. And I think, Oh my God did this just literally crush our baby's head. And I was so scared at this point because people are looking clearly this was not supposed to happen. Right.
[00:55:24] Jennifer: And then I remember [them saying], "It's okay. It's okay. It's okay."
[00:55:27] Lisa: They have a three popoff allowance.
[00:55:30] Jennifer: I was aware for the popping off and I was aware of her saying like, "it's okay. It's okay. It's okay don't worry."
[00:55:36] Zach: And Jenn to this day, doesn't remember this. And it's unfortunate cause she didn't have a mirror. And if she had a mirror, she would have known, I assume she knew how close it was. 'Cause I could see half the baby's head is out of her.
[00:55:46] Jennifer: I didn't have the energy to, to ask, even though it was on my birth plan and I'm pretty sure like written in the room, like "mirror for pushing."
[00:55:54] Lisa: You shouldn't have to ask in those moments, that's why you wrote it down.
[00:56:00] Zach: So she does these three pushes of 10 seconds. And it's clear at this point, after that third push of 10 seconds where she would normally then take a break, the baby was right there, that another push was going to get it out. So they make her do a fourth push at that moment, which she wasn't expecting. And she had no idea where things were. So she screams at the top of her lungs, "I'm going to die."
[00:56:22] And she doesn't remember doing that. Of course that fourth push. Got the baby out and I'm actually so glad I think we may have gone over this in class. I think I also read this in a book. That when the baby comes out, he's purple. He looks frankly to be candid, not alive. And that was very freaky to see in person because you look at it and you think something has gone wrong. I tell myself in that moment, intellectually, this is okay, he's going to be okay. And of course he was, and the color restore to his face and his body and he was fine, but it was very scary to see something that frankly does not look alive come out.
[00:57:06] Jennifer: At this point they put them on me for like, I dunno, a couple seconds. And then they whisked him away to the little table that they have in the room to do all of the, you know, take the snot out and put the things on the thing on their eyes.
[00:57:20] Lisa: And Peds was probably checking out the head to be sure there was no lasting harm as well.
[00:57:26] Jennifer: Yeah. I was really disappointed at that time because, you know, I thought that I could advocate for having him on me. And they just like, basically like ignored me the nurse that was taking care of him. He kept saying like, "Can I have him now? Can I have him now? Can I have him now?" And she just literally ignored me. And I was getting stitched up at this point, which was extremely uncomfortable.
[00:57:46]You know, the placenta came out, which was another thing that I wanted to see. And I just remember them saying, "Placenta's out." And then like, they discarded it. And I was just kinda like the baby's over there they're stitching me. This was really painful. They weren't telling me what was happening, you know, with my stitches, it was just like, they were like, okay, let's do a stitch over there.
[00:58:04] Let's do it. And so that was awful. And Zach kept coming over to me. And I kept saying, go to the baby because he is lonely. And like, he needs you. And we were talking and singing and, you know, Zach was like, I made him stay over there.
[00:58:17] Zach: Just to expand on that, I thought it was kind of a beautiful moment. I mean, obviously Jenn was going through a lot at that moment. And, you know, frankly, I was concerned about her. I had just seen her go through a pretty traumatic experience. I saw the color come back into our baby. So I'm like, okay, he's going to be fine. But her motherly instincts kicked in almost immediately. And her first and only concern was that I be there with our boy just to keep him company. And it was In my view of a pretty beautiful moment in the midst of chaos.
[00:58:46] Jennifer: Definitely. And I remember one of the nurses was like, what's his name? And I was like, I don't know. I haven't seen him yet.
[00:58:54] Lisa: Can I please see him?
[00:58:55] Jennifer: Yes. We have a video of Zach putting on the first diaper fumbling with the first diaper, which is really sweet. And then eventually I think I got him, I don't know, 20 minutes later, maybe 30 minutes later. So we had some time together and I wanted to start breastfeeding. So the nurse and the doula helped me a little bit with that. And he latched right away, which was great considering all the other things that didn't go the way I wanted it to.
[00:59:20] I was able to breastfeed. And then Zach packed up all of our stuff, deflated our birthing ball. And we went to the postpartum unit. They wheeled me in a wheelchair. And I got to carry the baby, which I thought was really, I felt like a queen. And then we went to the postpartum unit where I did not feel like a queen anymore. We really wanted a private room, but there were none available. The room that we got to. There was nobody there yet, but somebody, another couple came shortly after.
[00:59:47] Zach: So yeah, I'll jump in on this point here. And I think it's important for your listeners to think about this because obviously the biggest part of pregnancy or the end of pregnancy is the birthing process and being prepared for that.
[01:00:00]But you should be prepared for, you know, a lengthy stay afterwards and how you're going to endure that because you're not talking about staying at a five-star resort out in Telluride or something. I can't speak for every hospital obviously, but you know, in our experience we shared a room with another couple.
[01:00:20] So now you got to remember, you have a newborn that, you know, if this is your first child, you don't have any idea what you're doing. And then right next to you, separated by just, you know, a thin curtain is another couple with a newborn who has, you know, is crying also. So you're going to have constant interruption there. You know, one bathroom sharing with, you know--
[01:00:38] Jennifer: With no lock on the door and the husband of the other birthing mother walked in on me when I was in there. So that was awesome. At that point, I didn't even really care. I was like, you want to walk in this, well be my guest, but I would not want to be you right now.
[01:00:55] Zach: And then, you know, going back to what you were talking about earlier, the partner perspective here. Jenn had a bed, which, you know, did not look particularly comfortable and there was no bed for me.
[01:01:07]There was a chair, which was not particularly comfortable. Like an upright chair. So I, you know, we were there for two straight days afterwards, so I frankly just slept on the floor. And the hospital wouldn't give me any pillows because I was not admitted as a patient.
[01:01:24] Jennifer: Luckily, we brought some.
[01:01:26] Lisa: They often don't even have extra pillows. Which I'm like, how can you not have extra pillows?
[01:01:32] Jennifer: No, they do. Because people like us. Plan ahead and bring pillows and blankets, and then we leave them there. I'm sure everybody does that. I mean, a lot of people do that, so they definitely have accumulated some of other people's pillows, whether or not they choose to use them as another thing.
[01:01:47] Zach: On top of that, you know, this is obviously personal to us, but they happened to have been doing construction in a room, literally next door with drilling.
[01:01:55] So now you had in the middle of the day, really just pulsating, terrible drilling in the room next door. Obviously this is a complex situation where, you know, hospitals have budgets and people are coming in all hours of the day and night. It was actually surprising to experience something like this. I thought in a city like New York you know, mothers and fathers too, would be given more comfortable accommodations after going through something as traumatic as this, and really it's, you know, much worse than I think, than, you know, typical accommodation would be for, let's say, you know, an outpatient procedure or something like that. So it was certainly very stressful, just being there after the birth. And we were basically on a mission. I was more on a mission to get out of there as fast as possible.
[01:02:44] Jennifer: If you want to leave, start that process really early.
[01:02:49] Zach: Advocating for yourself and through the birthing process it's important to advocate, but the post birthing process is important to advocate as well saying, you know, I don't want to be here basically as a prisoner, please do what you need to do.
[01:03:00] And there are important things they need to do. They need to make sure the baby is healthy. You check all the boxes, the hearing, the vision, all that, but you know, there there's also a backlog and if you don't advocate, you may have to stay another day or two because they just never get to you. But I was in their faces and come on, let's get this going.
[01:03:19] Let's get this going. And if there's something wrong, we'll stay of course. But let's do the things we need to do to get to that point.
[01:03:24] Jennifer: Yeah,
[01:03:25] Zach: definitely wanted to get out
[01:03:26] Jennifer: of there as soon as we could. The nurses were, some of them were better than others. Some of them just like completely ignored, like what you said. And you had to really, I had to say like, can I have another ice pack? Sometimes I had to go into the hallway, which I didn't want to do and be like, "Hello, like nobody's answering the call button." Or if they do, they're really grumpy about it. And somebody takes like a really long time to come. The baby had this little like bassinet thing and, you know, I was kind of just like, I couldn't sleep.
[01:03:51] I'd probably slept like an hour the whole time I was there. Cause I was just like, there was a baby here and like, you know, we were uncomfortable and I knew I wasn't going to get much rest anyway. And I was just kind of like looking at him the whole time adoringly. They did take him for a couple of different things.
[01:04:05] Like he had his Hep-B shot in a couple of different tests and assessments and stuff like that, but he was doing really well. And they would come in and check on me with my vitals and make sure that he was doing okay. And was And then we really wanted to get out of there as fast as we could. So there was some videos we had to watch, like post-partum videos and, you know, baby care videos.
[01:04:26]And he had a hearing test and then we were kind of like ready to go. We were packing up. And then we realized we didn't really know how to use our car seats. So I thought it was, you know, you just put the baby in and you buckle him, but it was a lot more complicated than that.
[01:04:41] Lisa: It feels harder than it should, yeah.
[01:04:44] Jennifer: The car seat is a little tricky. Luckily he was fine. It was more like us not knowing what we were doing. So we had somebody help us and the car seat had been like a saga afterwards. Just like he hated it. We hated it. And we don't use the car seat very much because we're New Yorkers and we don't drive. And the times that we go in Ubers, especially now, is not very frequently.
[01:05:03] So, we figured out the car seat. When we got home, we took an Uber home. We met up with my brother and his wife, now wife, who live in our building and we got to see them sort of at a distance. And soon after our families came and we decided to have them, you know, see him, but not touch him. And then we quarantined for two weeks before we let anybody sort of hold him. And that was also a big conversation.
[01:05:27] Zach: Yeah. And I think to expand on that and it could be helpful for some of your classes is when you talk about kind of, you know, post-delivery things in this world today. The COVID discussion's a tough one. We've had many discussions and I think a lot of families are doing a lot of different things.
[01:05:42]I think we all recognize that, you know, grandparents and close family. I'll use the term-- I think one of the doctors said that there's a special relationship there and we don't want to preclude them from having access. On the other hand, we want to protect him and protect them because I think frankly, the irony is, I think they're probably at a greater risk than he would be.
[01:06:01] Jennifer: We knew that we had been, you know, most likely exposed to COVID in the hospital. So our parents are not young and we wanted to make sure that we kept them safe.
[01:06:10] Zach: I'm going to be honest, it's been a source of tension between us at times. It kills me to see, you know, my parents, my mother in particular loss both of her parents in the last year.
[01:06:19] So it was so important to me and is still so important to me that she, you know, gets to have the full experience with him. And right now we do allow them around him. We allow them to hold him, but we require masks. You know, we evaluate, I think week to week, month to month on when, or if that'll change.
[01:06:34] Jennifer: Things seem to be getting better, so we were sort of starting to think about re-evaluating that, but as things got worse, again were sort of sticking with the masks.
[01:06:42] Zach: And I think it's personal to every family. I think even talking to doctors, we've had some of our doctors say, "Babies do just fine. Like now New York's doing well. Yeah, you should let the grandparents kiss and whatnot." We've had other doctors say, "Oh, I don't let anyone around any of us without masks." And we have people in between. So I don't know if there's a right answer. You know, it's about everyone's assumption of risk, what they feel comfortable with. But I think a lot of families, it's maybe a silent thing going on with a lot of your clients now. I think a lot of families are going to have tension with people as people take different--and I'm not saying one person thinks masks are fake and the other think masks are real-- I'm not even saying that. None of us subscribe to the theory that masks are fake and don't do anything. But even within that there's nuanced differences on how much access people believe families should have.
[01:07:34] Jennifer: And everybody is acting differently themselves in terms of our comfort levels, being around them. Like some people are going out more than others and some people, you know, are staying home completely. So. It's also, you know, different within that.
[01:07:48] Lisa: I've seen more and more students coming to class on zoom that is, and comparing notes on like, how are you handling things with the family? That's a really important topic to think about and to compare notes on. And thankfully, so far, I haven't gotten a vibe of like judgment on the part of anybody. It's just been really supportive of like, yeah, it's a very personal decision, particularly because we're still early enough on, in the knowledge of this virus that so much of it is just conjecture and like, we're not fully sure what the right thing is to do, you know? So I'm glad you're touching on that because it is important to think about and be sensitive to for our family members and ourselves.
[01:08:30] Jennifer: It was something that was so important to us and we really didn't agree and we had to sort of come to some sort of compromise and, you know, continue to reevaluate and reflect on what's already happened. I did talk to a lot of people that I know that have young babies and children, or you know, older people who have grandchildren and really interviewed, like everybody that I knew to sort of be like, what are you doing? What do you think? And everybody feels differently. So you just kind of have to go with what you feel.
[01:08:56] But I do notice that the baby, and this is really sad. The baby does look at you differently when you're wearing mask and when you're not, which, you know, if you can't see the lower part of that grandparent's face it really sucks. Because it is such an important part of getting to know somebody is seeing their expression.
[01:09:13] Zach: So, you know, over time, at least, you know, sometimes we let them closer without a mask. Yeah. A little bit of a distance so they can, so the baby could see their face recognizing that it still takes time for a baby to be able to see further and further. But as of now, when they hold him or up very close to the space, they wear masks.
[01:09:31]We do a lot of FaceTime. We like to do it that way. So but I'm not going to lie. I'm sure. You know, as I said, Jen, and I disagree a little bit on the lines here, but I think we could both agree that it is a sad thing that the baby can't be kissed on their face by the grandparents or see them clothes up without the mask. It's heartbreaking, but we'll all hopefully get through it and get to a place where this isn't necessary anymore. I hope in the not too distant future.
[01:09:56] Lisa: Let's hope so.
[01:09:58] Jennifer: So the first couple of days we brought the baby home, everything was going really well. I had colostrum and I was continuing to breastfeed.
[01:10:05]It was really hard the first couple of days. And I recommend that your students definitely get help if they feel like they are having a hard time right away, especially at the beginning. Definitely there needs to be like a lot of like pushing through, but also like knowing when something isn't right. I definitely went and saw the doctor very early on. I had a lactation consultant come, and then I know you wanted to talk about circumcision. We kind of made it like a last-minute decision with the circumcision. We were going to have our doctor perform the circumcision, but she wasn't around.
[01:10:37]So it's going to have to be with another doctor at the practice. The doctor that delivered me, who I didn't feel too fondly about after everything that had happened. That doctor and I did not get along. And I just didn't feel comfortable bringing him to that practice to have him be circumcised after the way that I was treated.
[01:10:54]Also knowing that in the hospital and in the doctor's office or wherever you have your circumcision, you're not allowed to be present, which I didn't know. That my doctor's office would have made us wait outside. Because frankly they don't want to have to take care of us, which is what they told us.
[01:11:10]It's a very hard thing to see. And I sort of had a last minute change of heart. I think this was like a couple of days before he was eight days old, which we're Jewish. So the tradition is to have the circumcision eight days after you're born. Zach actually was in the NICU when he was born, so he had to have his at six weeks, but generally it's eight- day- old procedure. So I immediately reached out to my friend who works for a Jewish organization who sent me a list of mohels in the area. And contacted, like emailed as many as I could when they, and finally we got an email back pretty immediately from one of them.
[01:11:44]He was also a doctor. So I think that that really helped us. We weren't too sure about the mohel thing. Like the tradition is like, you know, this big Jewish guy comes over and he has a knife and you know, that was what my brother's bris was like, that's what Zach's bris was like. And you know, the mother is like screaming in the other room, crying.
[01:12:02]It was not something that Zach wanted to do. It was something that I felt was important. Obviously it's a very hard decision to make. Especially when you feel differently in your sort of thinking about the traditions of your people. And, you know, somebody said to me before I gave birth, well, if he's not circumcised, he's not actually Jewish.
[01:12:21] And to me, that was just kind of hard to hear, but an opinion. There are Jews that aren't circumcised, but it was a really tough thing. And I think my family, especially, and your family, actually, even though your family is less religious. We, they all felt like this is something that you should do.
[01:12:37] Zach: I was in the real minority of everybody here about it.
[01:12:39] Jennifer: Zach actually didn't want to do it. And if I agreed he would not have done it.
[01:12:44] Zach: Where I come from with most things in life, not to get too philosophical is I tend to not judge people for their views because I think the world's a very nuanced place. So that's my philosophical statement. Thinking about the act of circumcision for me, I think if there were no sort of historical tradition and someone started up a new tradition right now where we say, "Hey, we're going to cut off the tip of a boy's penis because that's our new religion. We'd throw them in prison."
[01:13:11] Lisa: Right. That's an interesting point.
[01:13:14] Zach: So it bothers me that we rely on history and tradition for something to me that makes little sense. I understand there's medical studies out there about some benefits of circumcision. I'm not here to debate those. I think you can debate a lot of it, but you know, I understand that there is literature out there on some of that.
[01:13:36]But the act of removing part of someone's body without their consent really does bother me. Especially that part of the body. Of course, there's also studies the other direction that say you may be removing some of their pleasure later on in life. Let's be honest.
[01:13:49] I can't know; I was circumcised as a baby. I don't blame my parents for doing it. And hopefully he doesn't blame me for agreeing to it. But suffice it to say it does bother me on some sort of intellectual level that we did it. And then on top of that, the actual procedure, I was holding his legs down and watching it.
[01:14:07] And I guess I was a little ignorant here as to the actual procedure. I learned a lot in your class about, you know, the actual birthing process. So not a lot surprised me there, but I thought the circumcision -- snip, snip, done. He cries, you know. But there's actually multiple tools involved and it's a pretty--
[01:14:26] Jennifer: He had a whole array of tools and he set up on our desk over there. It was like, we were just like, what
[01:14:32] Zach: It's a pretty grotesque procedure? And I watched a little bit. Other than when Jenn was in that distress, this was the queasiness moment for me of this whole process, watching this be done. And then yet he was happy, kind of smiling in a gassy newborn way. And then this happened. The convulsions that came over him and afterwards, to see him in that pain, I was tearing up. Every one we had a virtual zoom for everyone watching
[01:15:01] Jennifer: Immediate family.
[01:15:02] Lisa: I was just about to ask were you in your home?
[01:15:04] Jennifer: We were in our home. So it was the three of us and the mohel and then everybody else was on Zoom. Before we decided to hire this mohel in particular, we had a call with him and he explained that and, you know, I'm sure this is a selling point for him. This was not cheap. But he explained that circumcisions done in hospitals.
[01:15:22] Like it's done in a back room, they strap the baby down. The baby's screaming. They're all alone. When you do a circumcision, that is a bris, you can be with them. You can talk to them, you give them, you know, wine, which was my job. And, you know, it becomes a nice family, you know, tradition that you're bringing down.
[01:15:39]We would give them a Hebrew name, which we decided on Avraham Simcha, he's named after both of our grandfathers who are war heroes. And we each got to talk about our grandparents when there was a particular time when the mohel said that you could speak about the people that he's named after.
[01:15:56] So we did that intentionally to sort of like ease the experience a little bit and, you know, to humanize it or to make it a little bit less painful for us because I did want to do it, but I also wanted Zach to feel comfortable and as happy as he could about it. So we did, you know, have these lovely names
[01:16:17] Zach: Also as a little bit of a sidenote, as I indicated a little earlier in your podcast, my grandfather had passed away in the last year and passed away during COVID. So we couldn't have a funeral. He was down in Florida. No one could be there with him when he passed away. And this was a moment to be able to say some words about him since we couldn't do anything. And on a lighter note, you know, I kept saying to our boy, "You're doing so great. You're doing so great." Everyone on the Zoom call kept telling you after -- they think I was just comforting myself because I was so upset about it, that I was, you know, saying, "Zach, you're going to be okay watching this happen." But everything turned out fine. There is a lot of post circumcision care, you know.
[01:16:57] Jennifer: It's not easy to change diapers in the very beginning, when you have the circumcision care. I wouldn't change the diaper without Zack. I needed his support because it's hard. There's a bandage on it. And like, you're not sure whether the bandage is supposed to fall off or not. Our mohel gave us a whole sheet of instructions.
[01:17:15] He talked to us for probably like 45 minutes about the care. And then he said, you can call me anytime on the night, we still were like, "uh, like, we don't know what to do." And this is obviously such a sensitive part of your body, but. And it was hard to see. Yeah, it was hard to watch and that was a really tough part, but it definitely got easier as time went on and you only really do the care for about eight days. And then it's healed. On top of coming home for the first time, on top of COVID, on top of having a newborn and trying to breastfeed, you have this additional thing which, you know, I remember asking my dad about it and he was like, yeah, it was no big deal. And I'm like, It seemed kind of like a big deal to me. It was tough, but we got through it. Everything's fine. He doesn't remember. And if there's any silver lining, he went and got his two months shots two weeks ago. And it was like nothing compared to what he experienced during the circumcision. So my friends were like, "Oh, they're going to scream. They're going to cry. They're gonna scream like you've never heard before." And I'm like, " I've heard worse." They all have girls. Yeah. One silver lining, but I think overall I'm happy it was done. I'm happy that we picked somebody that was a doctor also a mohel. You know, somebody who we spoke to beforehand who we really trusted, who was just like a super nice guy. So if you need the recommendation, I can give you his name.
[01:18:34] Lisa: I was just about to ask. Yeah. I'll be sure to include that in the show notes.
[01:18:37] Jennifer: His name is Dr. Jeffrey Mazlin, and he was wonderful.
[01:18:42] Lisa: Great. Well, so as we start to wrap things up, are there any things that you haven't gotten to share that you would like to share, or as you reflect on this whole journey and how differently things went, particularly in terms of the birth itself are there any things that you would do differently next time or just any reflections, any insights for people who might be listening, who are expecting a baby?
[01:19:05] Jennifer: I guess go with your gut for sure. And just try to remember everything you've learned.
[01:19:11] Zach: I think I would say remember to advocate for yourself, which is something you teach Lisa. And not just in the treatment, right? The treatment obviously is the first thing you think about, but also in the things you want out of the experience, as Jenn said, she wanted a mirror, she didn't get the mirror. Perhaps more explanation of how things were going. Obviously postpartum advocating for the tests to be done so that frankly, you can get home and comfortable again, people can be there for you. So advocate, but at the same time, being ready to be flexible and adjustable to the circumstances around you.
[01:19:47] If you convince yourself that as long as you advocate for what you want, things are going to go the way you expect. I mean, I've only witnessed one birth, but I didn't see it go the way we expected it. It wasn't just because of lack of advocating. But I think if you tell yourself it's okay, that things could not go according to plan that you'll get through it physically and psychologically things will work out better, whether it is getting an epidural.
[01:20:13] 'Cause I thought in Jen's case that did change the ball game a bit. And even if you don't want to get an epidural, you know, if you're going to do a completely naturally the whole way through. To understand that you're not weak because things change along the way. I think for me, as cliche as it sounds, I think it shows an act of empowerment that you recognize things have changed and you have the fortitude to say, you know what?
[01:20:39]I'm going to admit that things didn't go the way I want, and now I'm going to adjust to make sure I get to where I need to be the best way I can. And I think if you combine those two things: advocating, but realizing that it's okay if things aren't perfect, that's the best course of action to have a good pregnancy and a good birth.
[01:21:00] Lisa: I love that you said you're not weak if the plan needs to change. That's really poignant to me. Resonates. Yeah, that's true.
[01:21:11] Jennifer: Like, yeah, that's our story. Thanks for listening to it.
[01:21:14] Lisa: Thank you so much for sharing.
[01:21:17] Jennifer: And I hope this is useful to some other people. I hope we shared some nuggets of information and our experience, and I hope it helps others to have the birth that they want or the birth that they ended up having or whatever it ends up being. Just remember to be flexible.
[01:21:31] Lisa: Thank you so much. I do hope that we can meet in person someday down the road.
[01:21:36] Jennifer: That's how I would think now it'd be lovely.
[01:21:37] Zach: When we have our second kid, I think we know the doula we're gonna be going to.
[01:21:42] Lisa: Oh, you're so sweet. I would love to work with you if the opportunity comes up.
[01:21:48] Thank you so much, guys. Have a great day.
[01:21:52] Zach: Thanks, you too.
[01:21:53] Jennifer: Bye, Lisa.