Jane & Sam, New Yorkers who met in San Francisco, share the story of their unmedicated, physiologic birth attended by midwives in a Manhattan hospital and supported by a doula. A year or so into being married, they decide to try to conceive with hopes of having a baby in the Year of the Dragon as Jane is Chinese-American. To their surprise, they get pregnant immediately after removing her IUD. Given Jane’s background having previously worked for a women’s healthcare tech company, she had learned enough about the maternal healthcare system to know she wanted to strategically position herself for a safe, unmedicated birth and to be well-supported by a doula. Jane also shares a bit about her breastfeeding journey and being well supported by two IBCLCs to be sure baby is thriving and to support her when she had some temporary initial nipple damage.
Resources:
Sponsor links:
Free “Pack for Your Best Birth” Packing List (with free mini-course option)
East River Doula Collective (find a doula, attend our free “Meet the Doulas” event)
Birth Matters NYC Childbirth Education Classes (Astoria, Queens and virtual)
*Disclosure: Links on this page to products are affiliate links; I will receive a small commission on any products you purchase at no additional cost to you.
Episode Topics:
Introductions & Background
-Meet Jane & Sam: former students, new parents, tech professionals living in Queens, NY
-Their relationship timeline and move from San Francisco to New YorkConception Journey
-Deciding to start a family and removing IUD
-Quick conception and initial reactions
-Cultural significance: Year of the Dragon
-Finding out about the pregnancy in BostonPregnancy Experience
-Early symptoms: morning sickness, nausea, and vomiting
-Coping with food aversions and strong smells
-Staying active: gym routines and adapting exercise
-Weight gain and healthy habits
-Navigating pregnancy health: avoiding certain medications, managing a mild feverPrenatal Care & Advocacy
-Researching hospitals, OBs, and midwives
-Switching providers for a low-intervention, unmedicated birth
-The role of birth classes and preparing a birth plan
-Hiring and working with doulas (Bori & Jay)
-Employer support: paid leave and doula reimbursementPreparation for Labor
-Packing the hospital bag and “nesting” behaviors
-Planning for a low-intervention birth and discussing induction
-Monitoring baby’s growth and fluid levels
-Dealing with the emotional ups and downs of waiting past the due dateLabor & Delivery Story
-Early labor signs, Braxton Hicks, and timing contractions
-The “false start” and real onset of labor
-Family support: the “clown car” ride to the hospital
-Arriving at the hospital in active labor
-Laboring on the toilet, using nitrous oxide, and Taylor Swift as the soundtrack
-Hands-on support: counter pressure, massage, hydration, and emotional support
-The role of the doula and partner during labor
-Overcoming challenges: rapid labor progression, overlapping contractions, and fetal heart rate concerns
-Avoiding interventions: changing positions, skipping pushes, and successful delivery without suction or epidural
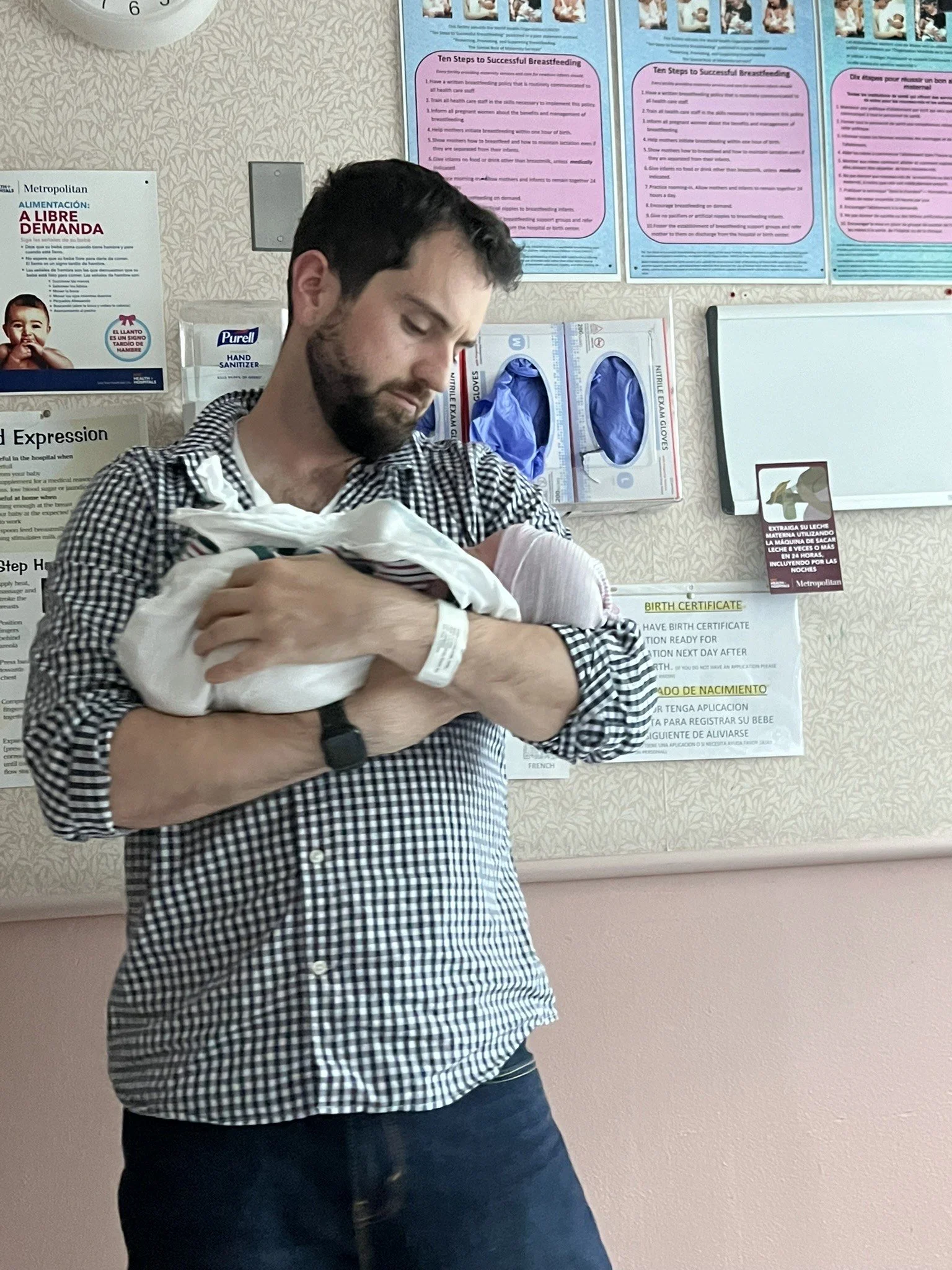
-The baby’s first moments: skin-to-skin, alertness, and first poopPostpartum Experience
-Immediate postpartum: emotions, exhaustion, and hospital stay
-Breastfeeding journey: initial success, nipple pain, and support from lactation consultants
-Learning to care for a newborn: diaper changes, cluster feeding, and sleep deprivation
-Navigating conflicting advice from nurses and finding confidence as new parents
-Emotional recovery: baby blues, anticipated nostalgia, and adjusting to new rolesReflections & Advice
-The importance of preparation, advocacy, and using available resources
-Lessons learned about paternity leave and supporting each other
-The value of being informed and having a plan
-Affirmations and mantras: “Pain with purpose”
-Final thoughts on the joys and challenges of new parenthoodHumorous & Relatable Moments
-Laboring on the toilet and the “hospital pillowcase incident”
-Taylor Swift as the labor soundtrack
-The “clown car” family hospital arrival
-Diaper blowouts and learning to tie diapers tight
-Honest confessions about sleep, snacks, and hospital food
Interview Transcript
Lisa (0s): You are listening to the Birth Matters podcast, episode one thirty three.
Jane (4s): I was screaming and sitting on the toilet,
Sam (7s): Screaming, sitting on the toilet.
Jane (9s): They had the nitrous oxide.
Sam (10s): We had just enough slack for her to sit on the toilet and have the mask on her face. Yeah, and that helped you a good bit. Yeah,
Jane (16s): We had Taylor Swift playing in the background. I think Sam associates that music now with me screaming my head off.
Sam (23s): Yeah, it's a really weird scene to have a woman who's screaming on a hospital toilet with Taylor Swift, singing about Boys in the Background.
Lisa (44s): Hey there and welcome to the Birth Matters Show. I'm your host Lisa Graves Taylor, founder of Birth Matters NYC, and director of East River Doula Collective. I'm a childbirth educator, birth doula and lactation counselor, and I've been passionately supporting growing families since 2009. This show is here to lessen your overwhelm on the journey into parenthood by equipping and encouraging you with current best evidence, info, and soulful interviews with parents and birth pros.
Please keep in mind the information on this show is not intended as medical advice or to diagnose or treat any medical conditions. Have you subscribed to the show yet? Please be sure to do that wherever you're listening to this or over at Birth Matters show.com so you don't miss out on anything. Today Jane and Sam New Yorkers, who met in San Francisco share their story of their unmedicated physiologic birth attended by midwives in a Manhattan hospital and supported by a doula A year or so into being married.
They decide to try to conceive with hopes of having a baby in the Year of the Dragon as Jane is Chinese American. To their surprise, they get pregnant immediately after removing her IUD. Given Jane's background, having previously worked for a women's healthcare tech company, she had learned enough about the maternal healthcare system to know she wanted to strategically position herself for a safe unmedicated birth and to be well supported by a doula. Jane also shares a bit about her breastfeeding journey and being well supported by two IB CLCs or lactation consultants to be sure baby was thriving and to support her when she had some temporary initial nipple damage.
And now a quick word from our sponsor, East River Doula Collective's. Next meet the Doulas event will be on Wednesday, September 17th at 6:30 PM on Zoom, and our next virtual savvy Birth one oh one workshop will be on Wednesday, September 24th at 7:00 PM on Zoom. You can find the link to sign up for either of these events on the top, banner over at Birth Matters nyc.com. So if you're expecting a baby or even trying to conceive, we'd love to see you at either or both of those events.
Also, our all-in-one childbirth class series are filling up really quickly for the fall. So if you're due in the next few months, be sure to grab your spot soon. We currently have dates posted all the way to the end of 2025. Also, just a reminder that If you don't live in New York City or you just don't wanna have to travel for childbirth class, we would love to have you join us for our live group interactive class series virtually on Zoom. A lot of folks have found this to be a very convenient option while still having the benefit of being able to chime in and ask questions in real time.
This format is also priced lower than the in-person option, so it's a great option for folks with a more limited budget. You can check out this option as well as several other childbirth class options like private classes or our online on demand course all over at Birth Matters nyc.com. Okay, let's jump in and hear from Jane and Sam. We share a lot of laughs in this episode and I hope you'll laugh along with us today. I have with me former students of mine, Jane and Sam.
Welcome. I'm so glad to see you again today.
Sam (4m 17s): Say thanks. Great to be here.
Jane (4m 20s): Thanks Lisa. Great to be here.
Sam (4m 22s): Yeah, thanks for having us.
Lisa (4m 24s): Absolutely. Could you please just start by introducing yourself a little bit? Maybe let us know how long ago you gave birth, I know it was very recent and where you live and anything you'd like to share.
Jane (4m 35s): Oh, hi, I'm Jane. I gave birth a month ago and we both live in Woodside, Queens.
Sam (4m 41s): I'm Sam, I observed the birth a month ago. We should maybe say something about our background. We've been married for how long? It's gonna be in four years. It was
Jane (4m 50s): Two years when she was born.
Sam (4m 52s): Two years when she was born. Okay. But we've been together for, it'll be five years later this year. Yeah. And we met in San Francisco. We're now in New York. We both work in tech. Jane's in a kind of sales operations role for a really big company. I'm in a salesperson's role in a very small company and yeah, it's been great. It's our first kid.
Lisa (5m 16s): Nice. Congratulations. So why don't we start with your sharing anything you'd like to share about your conception journey and then going on into how your pregnancy was.
Jane (5m 29s): Yeah, I think we had it fairly easy. I was on an IUD birth control prior to our conception. Prior to trying to get pregnant, we, like, I took it out and then the next month, like we tried and we got pregnant instantly. So we were fairly lucky. I almost was a little nervous because I was like, wow. Sam was like, oh it takes six months on average to get pregnant. And I was thinking that like I know my body, I feel like I'm gonna, it's gonna be happening really quickly. And so it happened like the next month and wow.
I was sad because I was like, oh my god, I didn't even get sushi in for the last time before getting pregnant and I had to stop. So that's the priority. Yeah. I was like, I have to stop the sauna. We were like going to the gym regularly and doing the sauna and obviously when you're pregnant you can't do the sauna, especially in the first trimester. We were excited but also nervous at the same time. It was just, it happened really fast. We did the first response like they, they have the three tests like the early, like early and then the regular test and then the confirmation one and then when we did the early one it was a negative, but then after like the day I missed my period, I did the regular test and then it said it was pregnant and I was like, oh my god, this is crazy.
Yeah,
Sam (6m 45s): We have a little more detail than that. Right. We were gonna start trying, this is the year the dragon Jane's family's Chinese. It's a good year to have a kid and lined up with about what I was expecting as well: stay, get married a couple years in, have your first baby. And Jane got her IUD out and I was expecting it to take months. We were gonna aim to have a kid in like, conceive around October. I was like, we may as well start earlier because it could take who knows how long really? And, but no, it was the very first month she got pregnant and we were in Boston and I was there for a conference and Jane came up to visit and it seemed like she was a little late.
We were like, ah, maybe we were pregnant. I was excited. But she took the test a couple days before, a day before it was negative. And I was like, ah, disappointed though. But then when she came and visited me in Boston, she took one and there it was positive. So that was pretty cool. Very exciting times.
Jane (7m 43s): I remember that moment vividly. I went to school in Boston so for me that It was like a special place to find out I was pregnant and it was, I lived like my first like early like adult years independently there. So It was like a funny coincidence. But I remember like I had a four o'clock meeting and I was like, okay, let me just pee on the stick before my four o'clock meeting. And then we had dinner plans like, we were gonna leave instantly at four 30. But then like after my meeting I looked at the, the pregnancy test and It was like pregnant and I don't know, It was like a big
Sam (8m 14s): Shock. You broke the news to all your friends and stuff.
Jane (8m 17s): It was really cool. We had dinner with our friends but we couldn't keep it secret. I know a lot of people were like, oh yeah, like we could keep it here. But we were like, oh my god, this just happened to us. And we were having dinner with like good friends and so we wouldn't, we weren't saying hey, we're expecting, it was more like, hey, we just got a pre a positive pregnancy test and we'll see what happens. But yeah, it was just, It was wild. A crazy experience. Yeah, yeah,
Lisa (8m 40s): For sure. So fast. So then what, then what, how did your pregnancy go?
Jane (8m 46s): It was, initially it was fine. Like when I instantly got pregnant or initially when I got pregnant I was like reading, I used to work in a women's health company and so like pregnancy, like the idea of doulas, lactation consultants, like C-section rates at hospitals. They were not new to me. So I was reading voraciously every book I could find. But then I got the morning sickness and then I was really nauseous. I was nauseous for a few weeks but then the throwing up came in and
Sam (9m 18s): The first time we threw up we were actually in Taiwan and then we were like, oh she hasn't thrown up yet. Like maybe this is gonna be an easy pregnancy. And then we were walking back from dinner and it was just, and then we were like, uh-oh it begins. And then sure enough it began. Yeah. And from that point on, Jane was quite sick, quite miserable. It was a pretty rough first trimester.
Jane (9m 42s): I was so tired. Like the worst of it. I think they say nine to 10 weeks is the worst of the nausea and like vomiting. Yeah, like that. Around that time it was like throwing up three times a day and I think we had a road trip during that time as well and I had some Ziploc acts.
Sam (9m 60s): Yeah, she was like puking in a, in a used pork grind bag. Like everywhere we went we had to think ahead, okay, what can you puke in?
Jane (10m 9s): It was so true. We would go to like gift shop and be like, they're like, do you need a bag? We're like, no. But they were like, oh wait, we might need a bag, do you have a plastic bag? Like that'd be really great. We could just take it with us and use it as the emergency bag. Yeah,
Sam (10m 23s): She was pretty miserable also. Like she used to pride herself on never throwing up and prior to this she's like, I'd never throw up. 'cause every now and then, you know I might get sick or something. Right. And boy she threw up enough, probably 10 extra.
Jane (10m 37s): Yeah.
Sam (10m 37s): Throw up in your life.
Jane (10m 39s): Think I could count on one hand prior to that the number of times I threw up. But then really?
Sam (10m 44s): Yeah, she was pretty miserable. Like she really did not enjoy the first trimester and I tried my sister and other people we know. Yeah, it gets better. Jane has a thing and this happened in different stages of the pregnancy where she has a hard time believing anything is going to get better when it's happening to her in the moment. True. And that repeated itself in different ways throughout and after the pregnancy, but she keeps being proven wrong. Everything bad that happens keeps getting better. So maybe she'll internalize that at some point.
Jane (11m 11s): Yeah, it slowly got better. I used to throw up three times a day and then it would be like one time a day and then it would be like one time every few days. And then like once a week I tried to eat healthy and stay active during pregnancy. But that was like during that time it was really hard. Like I just ate what I could. Oh absolutely. I think there was a time where I was like eating crackers every like 10
Sam (11m 35s): Minutes you ate it smells. Oh
Jane (11m 36s): Yeah,
Sam (11m 37s): We eat pretty healthy here Jane. I will stay to her credit and maybe we'll get more into this. I think during the pregnancy Jane did a lot of things really. She stayed away like no caffeine, no alcohol. She stayed away even from stuff that's not contraindicated but some people think is risky like Tylenol and ibuprofen even. And she, yeah, she did stay very active but there was stuff that she just couldn't handle. Like smells, any kind of cooking smells, cooking meat, cooking oil, couldn't handle it. I don't know. Have you had chicken yet? You got turned off a chicken during pregnancy?
I don't, I think
Jane (12m 9s): It's handle, I first tried It was like making Greek lemony chicken soup and then I was handling chicken and then afterwards I just did not wanna like ever see chicken again. There was a picture on Sam's phone where I like was peeling an orange. I put the orange rind on my nose because I was just like trying to, the clean smell helped me. But like cooking smells just made me puke. I think I went to the office a lot even though I can work from home but because the office is super sterile and it doesn't have a lot of smells. So that was really helpful I think being outside and just not staying home all day.
It
Sam (12m 41s): Was and kept up at the gym. Like you were very pre, you were still very pregnant at Equinox. I remember seeing her bouncing on the ball. Her stomach towards the end was almost as big as the Swiss ball. She's bouncing on and she did a really good job. I think staying active. She, you gained a lot of weight but like you were still like, it seemed like you were almost quite lean. It was all like a healthy weight. I feel like that you gained, I
Jane (13m 4s): Have gained almost like 40 pounds. I know that's like the upper limit normally. I mean everyone's different right? It's healthy, normal. Yep. Everyone's different. Yeah. But
Sam (13m 13s): I feel like that helps the baby. I was like everything we were doing. It was like how is this gonna lead to the best baby and like how do we avoid bad things? And I think we pulled it off. She's a good one.
Lisa (13m 27s): Score
Jane (13m 29s): Goal achieved. Yeah. I wasn't drinking caffeine anyway and I know people don't take ibuprofen. You have to take Tylenol. I didn't get too sick during pregnancy and so it was when I did, I tried to, I tried to avoid, there's certain things like I'm sad that there's not, it's not like a, you can still take it when you're pregnant but where I could tolerate it, I try to like could have open taking
Sam (13m 51s): It. There was one time when we both got sick, we both got a fever and it was scary right? 'cause it's okay fevers, you hear horror stories. But Jane got over it. It was like a very low fever. We kept watching for it to tick over. It was a hundred, 101.5 or something when it's okay now you
Jane (14m 6s): Know
Sam (14m 7s): Four you gotta handle it. Yeah. And she got very close and then like almost at the end and then she didn't quite get there and then she got better. And then meanwhile I got way sicker. It was miserable for a week. So, that was the only thing that happened. And then of course Roland talking about the negative stuff but there's lots of positive things, like a lot of positive moments. Getting the first sonogram back, seeing her little face later in the pregnancy. Which you would look at all the time for motivation. Yeah, for sure. Like we got one really great sonogram shot that showed her, maybe we'll share it in the follow up but showed her little face and her face actually ended up looking pretty close to that sonogram.
And so Jane would like look at that picture to try to keep her eye on the prize, right?
Jane (14m 51s): Yeah, for sure. Actually that sonogram we, they measured her size on that one and she was like 10th percentile. And so that was like a scary moment during pregnancy where 10 percentile was like the kind of cutoff right below that. It's like there is potential or there is fetal growth restriction. And so we had to get additional, we waited four weeks to get another measurement of her. At that point she was like 20th percentile. So that made us feel way better because initially we were concerned, we're like we've never been 10th percentile in anything in our lives.
So It was like we were a little concerned.
Lisa (15m 28s): You achievers overachiever.
Sam (15m 31s): Yeah. And Jane Swap too. So she was going to an OB who was fine. There's nothing wrong with it really. Yeah. But she, we were doing more research and then of course we went to your class and got an additional perspective which was helpful and great and I think it was before we started gonna Lisa's class you swapped to Metropolitan. Yeah. Because they have a low intervention rate and they have midwives. Yeah. Yeah. And that ended up being I think a really good decision.
Jane (15m 60s): Yeah, Lisa actually you gave me, I reached out to you in that form before we attended your class so we felt super lucky that we were able to make that change earlier. The way I found the first OB was I was like on Zocdoc and I was overwhelmed. I was like I just need to find someone I can, I made a few calls but then there were like, some appointments are hard to find and I just found someone that could be easily accessible to me at that time. Like he was close to my office. It was easy to make appointments with him and so I just went with him for a bit and I knew that you could change providers later on.
And then when I reached out to you to provide my kind of pre birth preferences, you gave me some options. I think Oula was one of them. Metropolitan was another. And then I think Central Park midwives, I think that one at that point they were already booked 'cause they're in such high demand. But we looked at Oula and Metropolitan and ultimately I think Metropolitan was the kind of right place for us. And then also at that time you gave us, I was, I told you I was interested in hiring a doula and so you gave us some options as well.
We ultimately, we interviewed a bunch of people but ultimately we decided to go with Bori and Jaye who are amazing. We think of 'em as aunties for Audrey 'cause they were there supporting us before her birth and then after her birth during, during her birth and then after her birth. So it was, it was a great experience. We actually miss them a lot. Like we still like text with them all the time. We still do, but yeah, it's a little different now 'cause she's here.
Lisa (17m 33s): Sure. A little trickier or a lot trickier. Yeah. I just spent the last two days with Jaye 'cause we did a spinning babies two day class with a whole bunch of l and d nurses from NYU. So it was really fun to get to hang out with her for longer than I normally get to. Wonderful. Yeah. I'm so glad you had their support and I'm glad that you were able to switch to a provider that felt more aligned with what you're, what you hoped for. Do you wanna give any more context in terms of what kind of birth you were hoping for more than you already have?
Jane (18m 6s): Yeah, we were aiming for an unmedicated birth. I know a lot of friends who wanted to do that but then ended up going with epidural or other, their situation necessitated another path. But that was what we were going for. We were like, okay, like we're obviously gonna do whatever is best for me and the baby. But at the same time, like after reading and looking at some of the research we wanted to go with the unmedicated birth, we wanted a low intervention birth and I think that that dictated where we wanted to go.
I think you said a lot of great things about Metropolitan and then that also played a part in the decision of the doulas that we wanted to hire as well. Like we wanted to hire people who were experienced in that and then or and aligned with that vision.
Sam (18m 52s): I don't know if we're probably gonna get to the exciting stuff, right? The actual birth, which was interesting and I was there for the whole thing. A lot of observations on that but yeah. But ultimately, you did pull it off, spoiler, l so I guess we could talk about that. Yeah. Oh, whoops.
Lisa (19m 6s): No, it's okay. Yeah. Were there any other things you wanted to share about your pregnancy before you jump on into your birth story?
Jane (19m 15s): Hmm. I think that's it. Anything else that you can think
Sam (19m 21s): Of? No, I mean you took off work about a week before you were due. Your work is awesome. They offer you six months paid leave.
Jane (19m 28s): Yes,
Sam (19m 28s): True. So that's
Jane (19m 29s): Sweet. Amazing.
Sam (19m 31s): Most people don't get that. And yeah,
Jane (19m 33s): There's a, oh I mentioned this earlier, but the doula reimbursement. Yeah, they actually gave a stipend for hiring a doula and so that was really helpful. I think I would've hired one anyway, but that just also just incentivized me further to do the research. And they also, the company that my com company works with on that gave us a bunch of questions to ask doulas. And so when we were interviewing doulas, those were some of the questions that helped us decide ultimately who we wanted to go with.
Sam (20m 4s): Yeah. And of course we did the birthing class with you, which was nice. That was really cool. Learned a lot. Yeah. And I, I think we had that hospital bag packed like a month in advance. That was the big thing. And of course you, you at some phase towards the end of the pregnancy definitely went into nesting mode, right? They always talk about that and you denied it at the time I was like, you're in nesting mode
Jane (20m 25s): Right now. I'm still denying it because I am just deadline driven. Like I have always been that way my whole life. Like I, there's a
Sam (20m 31s): Deadline I know maybe
Jane (20m 32s): And then I'm going, I'm working towards it. I, I
Sam (20m 34s): Think maybe it was a little bit of both, but we got all of that lined up and by the time the pregnancy actually, the labor actually started. I can't imagine being more prepared.
Jane (20m 43s): Yeah, I had your hospital pack packing list and I was checking off, It was like, okay, what do I need? Ultimately we didn't need everything and it was helpful. Oh yeah, no, yeah. Like see what we needed for next time we have another kid. But,
Sam (20m 56s): And we did the birth plan too. The doulas helped us go through what the birth plan is and made like a nice visual printout. Yeah.
Jane (21m 3s): I love the ones they use.
Sam (21m 5s): I've heard this too since then. People are like, yeah, I had this plan and the doctors told me to pound rocks and they didn't do what I wanted. And I think having it and also metropolitan to their credit that when we got there they were like, do you have a birth plan? And we were like, yes, here are three copies. And that was it.
Jane (21m 23s): Yeah, I think I also Bori, and Jaye recommended that I bring the birth plan prior to just one of my midwife appointments. And so I, I just brought it and then the midwives reviewed it as well. And so I think I knew what to expect when a midwife would look at my birth plan and so that was helpful as well. Yeah.
Sam (21m 42s): And then one day contractions began
Jane (21m 46s): Drummer roll. Wait, even before then, I think the midwives, like a lot of times I, this is what I hear and you probably know better than I do, but like a lot of when you pass 41 weeks, a lot of doctors wanna induce you. And I think Metropolitan was super helpful in that they were open to going past that. So I delivered at 41 weeks and two days. And so once you pass your due date, you have to go in every twice a week for the non-stress tests. And so I went in and the midwives then were measuring my fluid levels and I remember you told me like, Hey, just drink a lot of water for your appointment so your fluid levels look good.
I was just, yeah, I would also like, just was thirsty all the time. Like ice water was like my go-to beverage. Like I always had my ice water bottle all the time and they,
Sam (22m 39s): You were really tired of being pregnant towards the end. Maybe that's the last thing I'll say. Like after 40 weeks she was like, get this baby out of me every day. She was just, she was over it. She wanted her out. Yeah. And we thought 'cause it, when you actually did start feeling contractions, we only had maybe two days before the scheduled induction and we were debating, we were like, should we ask them to bump it out more? Like we don't really want to induce, but maybe we should. So we were going back and forth but fortunately it didn't end up being an issue.
Jane (23m 9s): Yeah. I think what scared me about being induced was that the contractions would be more painful and I wouldn't be able to get that like natural or like unmedicated birth experience. So you know, the midwives were really open to it. At least the main risk was that baby would have her first poop like inside me and that would not be optimal for birth more on her first poop later or to come of that. But that was my concern. I wasn't as concerned about some of the other aspects.
I just wanted to make sure that we didn't necessarily need to be induced for that.
Lisa (23m 49s): Yeah. And I, it is more common for a baby to do the meconium staining to poop in utero. The more mature they are, the later we go in pregnancy. But it usually isn't just for listeners who are like, oh that sounds scary or just what is that? Most of the time it doesn't cause a complication for the baby. It can and it is something to monitor more closely, but most of the time it's of no consequence. So I just wanted to clarify that. Yeah, again, that's not the most common concern I usually hear expressed by care providers in terms of letting us be pregnant for longer without needing to be induced.
So that's interesting to hear.
Jane (24m 25s): I, so I basically asked her like, Hey, if I'm not delivered by 42 weeks, can I, can you induce me then? And then she really recommended to get induced earlier because she said at 42 weeks that's where there's a higher likelihood of the meconium coming. But yeah, I think it's, from what you're saying, it sounds like there's different risks.
Sam (24m 44s): Yeah, she was a small baby, so in my mind I was like, I feel like she's just finishing baking, you know what I mean? She's not quite, she's not quite puffed up yet. And I think that I was right, I think it was right. I think she just wasn't ready to come out until she was ready. And then when she was ready she really did come out. Yeah. Should we sec, should we segue to that part? That's the fun part.
Lisa (25m 5s): Please do. Yeah, go right ahead. Yeah,
Sam (25m 7s): I, so what happened? What happened when your labor pain started? I,
Jane (25m 12s): I had Braxton Hicks contractions during pregnancy or during the later stages of pregnancy and they would get worse. Like sometimes in the morning I would, if I didn't drink water, I was, when I was pregnant, I was peeing up like multiple times a night. But then if I didn't rehydrate after going to the bathroom, I would have more Braxton Hicks contractions. That's like a trend I saw in myself. But then one morning I woke up and I felt like it was that like, you know, the repeating contractions that kind of got me thinking, hey, maybe I'm going into labor.
There were intervals and Hicks doesn't have that. And so I woke up and then I went to the living room to just start doing the contraction timing. And I could see that, oh, it was 20 minutes and then every 12 minutes. And so it was like the timing between the contractions got smaller or they grew shorter and, and then I like took a screenshot and sent it to Bori and Jaye and they were like, yeah, it looks like you, you may be going into labor. And then I think Sam woke up at that time to go on his run 'cause he's training for a marathon
Sam (26m 16s): Like every other 30 something man in New York.
Jane (26m 21s): And then I was like, Sam, I think I'm going into labor. And, and then we're like, oh my God, this is it. And then I did learn from your class and then talking to Bori and Jaye we, I know that I need to get rest, right? Because when the contractions are light, like that's when you should be getting rest. 'cause to prepare yourself for the later stages. And so I did that. I went to take a nap. They weren't strong at all. So I went to take a nap and then Sam went on a run. I
Sam (26m 47s): Went on a long run and I was like, oh man, this is the last run I'm gonna do for I'm a dad. I was like, my mind was racing. And then I got back and you were like, I don't know, the contractions have stopped. And then we Googled around. We're like, I guess maybe that was, was it prodromal?
Jane (27m 1s): Prodrome, labor prodromal. Like we were maybe like, oh maybe this, we got faked out by it. It wasn't actually labor. And so it was also my brother's birthday. And so we just went on our day. We're like, oh that's a bummer. I don't wanna get induced. Hopefully I'll go into labor. And then It was like
Sam (27m 16s): Nothing really. So that was like in the morning of that Saturday you started feeling them then they went away for hours and then
Jane (27m 25s): They would occasionally come here and there and it was my brother's birthday. A pretty week though. Yeah. Yeah. Pretty week. But then I was just baking a cake. I was like okay, I'm just gonna go on my day, just bake a cake, keep my mind off of it. And we
Sam (27m 39s): Were in our minds we were like, okay, it probably is gonna be days like if that's what it is, it's probably gonna be days and you might have to get induced. And it was a bit of a disappointment but it is what it is. And so we had a normal day and went to bed. But then when we went to bed, which would've been like nine or 10 that night, like you were like, I feel I'm starting to feel weird or what, what, what exactly
Jane (27m 59s): Was it? I was like, I don't think so, so Sam went to bed and I was like, I don't think I can sleep. Like the contractions at that point got stronger and they were not at the point where I can just sleep through it. So I was hanging out in the living room and timing my contractions every now and then. And they got more intense I think in the class. We learned about the 5 1, 1 4, 1 1. I felt like my contractions were getting intense very quickly. Like It was like 20 minutes and it was 12 minutes and then eight minutes, seven minutes.
And then it got to the point where It was really painful and It was like four minutes between fourish, minutes between contractions. I'm like, there's no way that I got there that quickly. Normally textbook is, it takes longer. And so I was like timing it. And at that point, every time I get contracted I ran to the toilet because I was, I just felt that sensation of I'm gonna make a bowel movement or something. And I was like, I don't want to kill for most of my labor. I was like laboring on the toilet. 'cause I was like okay, it feels good to be like here you, no, but I was, when I was in the apartment I was like running, oh I guess it was considered labor.
Yeah. I was running to the toilet every time I felt a contraction coming. I'm like, okay, running to the toilet. And then Sam was sleeping 'cause I wanted him to get rest 'cause I, I wanted him to be alert when we were in the hospital but at some point it was hard trying to like, I really wanted to be very vocal but I knew he was sleeping and it was hard to suppress that. But
Sam (29m 29s): You got me up, you got me up at about midnight.
Jane (29m 31s): Yeah. Yeah. And then I was like, Hey can you time my contractions? Am I going crazy or am I at four minutes between contractions, what was
Sam (29m 37s): The app you were using?
Jane (29m 38s): So it's an app called Ovia Pregnancy. And so that's actually the company I used to work for. And so I was using their app to, they
Sam (29m 45s): Have a contraction timer
Jane (29m 46s): To like contraction timing. Yeah. And at that point, oh Sam was like timing my contractions. And he was like, you're right, it's four minutes. And I think I called the midwives too as well. And then later the midwife was like, yeah I could hear your change in your voice. Like you felt very stressed out. I didn't know I was, at that point It was like having some self doubt. It was like, am I like timing this wrong? Like how did I get here so quickly? Am I like, do I just just have low pain tolerance?
So at that point,
Sam (30m 18s): No it was there. It was really obvious like yeah, it was really obvious. And also the sound. Yeah, the sounds you were making definitely changed. You went from, oh this is really uncomfortable. 'cause like earlier in the day, like we would go on a walk, then you'd be like, oh here's one you would stop and brace on me for a bit and then it would pass and we would continue this. You were like, oh. It was completely different. And It was like, oh man, this sounds like it hurts. And yeah they were pretty close together and that's when It was like all hands on deck. Yeah.
And we're in a very unique and interesting living situation. Right. We're actually in a triplex in Queens where Jane's mom and dad are on the first floor and her grandmother and brother are on the second floor. And then we were on the top floor. And so yeah, It was like all hands on deck and we got, we all loaded in the car. We got the,
Jane (31m 8s): It was more people than I, It was like a clown car. It was like Sam, I just needed my brother to drive me and Sam. But then my mom was also awake 'cause she just went to a wedding that evening. And so she's, I'm coming too. And literally It was like the most it could fit. 'cause we kept the car seat
Sam (31m 23s): Like and we got installed, got the kit we got, It was like three bags. It was like I had a bag, Jane had a bag and we had like an auxiliary bag with pillows. And so I'm loaded up and we go to Metropolitan. Takes about 10, 10, 12 minutes to get there. Not too long. Yeah. And what happened? Did the security guard just point or something and you just walked right by?
Jane (31m 41s): We, there's like a metal detector at Metropolitan and then he just saw me, we're in the middle of the night. I'm like groaning And so they're like, yeah go through. Like he didn't make Sam go through the metal detector.
Sam (31m 53s): Yeah, this happens all the time. And and we got up there and I guess the first thing that they did
Jane (31m 58s): Was, was triage. Yeah, triage. I think they like go check you out and see how Yeah, I feel like they hooked us up. Yeah.
Sam (32m 5s): We got in touch with the doulas also and the doula said, Hey, let us know when I think what five centimeters dilation or something like that. Five six. And they measured you five six and you were already there?
Jane (32m 14s): Yeah, I was at six centimeters or six five or six centimeters already. Which made me feel better. I was like, okay. Like I didn't, I'm, it's not just 'cause I have a low pain tolerance, like I'm actually, yeah, we
Sam (32m 27s): Were concerned about going there and then being told that you're not far enough along and then having to turn around and go back. So that was the big, big question. We were like, is this really labor? Like it seems like it is, but it's also weirdly quick. But it turned out to be very good that we went ahead and went 'cause it was real.
Lisa (32m 45s): Yeah. Yeah. That's a nice time to arrive in active labor. Great. Yeah.
Jane (32m 50s): And then
Sam (32m 51s): And by that point you were yelling?
Jane (32m 52s): Yeah, I was yelling. I'm not shy about vocalizing my pain. It got worse later on. So I think after they measured me there was more monitoring and stuff like that. I think they have, what is it, the continuous monitoring, but it's like without the wires so you can walk around the wireless, the wireless monitoring. So I got my own room and then at that point I just ran to the toilet. I was like, the toilet is comforting to me.
Sam (33m 21s): Yeah, the room was nice. It was like it's, there was a nurse in there the whole time. There was a bed, there was a couch and there was an en suite bathroom and Jane ended up spending maybe 90% of the labor in the en suite bathroom. So we got there at around maybe a little after, I mean 1230 or something like that. And you were in the room actively laboring by 12 45 1. And then the doula bore, she came, she was there I think less than an hour later and she started helping out, which was awesome.
Jane (33m 59s): Yeah. Part of me was like, Sam was really helpful and he kept me hydrated the whole time. He was like feeding me electrolytes and like water and, but it was just really great to have bore there. Like part of me was like I might poop. I don't, I like, I just didn't want Sam to see me. I know it's a weird thing but I was like, can you just go out and just, can you just wait outside by the, or like in the room. I was in the like the bathroom and
Sam (34m 26s): Paint. Paint the picture. What was happening right during the bulk of your labor? What were you doing?
Jane (34m 31s): I was screaming and sitting on the toilet
Sam (34m 33s): Screaming. Sitting on the toilet and, and we say unmedicated but the Metropolitan did have one option. Yeah. That you felt comfortable doing?
Jane (34m 41s): Yeah, they had the nitrous oxide that was there and initially they were like, oh you can't bring it into the bathroom. They
Sam (34m 48s): Were like, we don't think of that, that it'll even extend to the bathroom. And I was like, no. I was like twisted it around. I was like see. And then we had just enough slack for her to sit on the toilet and have the mask on her face.
Lisa (34m 60s): Nice.
Jane (35m 1s): Yeah.
Sam (35m 1s): And that helped you a good bit? Yeah,
Jane (35m 3s): We had Taylor Swift playing in the background. We had some music. Even though I think Sam associates that music now with me screaming my head off.
Sam (35m 12s): Yeah. It's a really weird scene to have a woman who's screaming in agony on a hospital toilet with Taylor Swift singing about boys in the background. It was very surreal, but that's what she wanted. We did
Jane (35m 28s): It
Lisa (35m 28s): And I just keeping it was
Sam (35m 30s): Watered.
Lisa (35m 31s): And with your screaming, I love the watering. That's wonderful. So important. And your vocalization was, what was it? Can you say more in terms of did it feel really empowering or were you in at all of a head space to like, I don't know, keep it in the low range or any of those things we talked about in class? I think, I think
Jane (35m 51s): I experimented with it. I think I would just try to make different sounds and like there were some like grunting and like, you know. Yeah. I don't know. I think I just went
Sam (36m 2s): There. It was very loud. I was surprised that metropolitan they, the hospital, they left the door open too because I couldn't imagine coming into the hospital for a checkup that morning or something and hearing like just blood curdling screams emanating outta this room. But that would be pretty unnerving. But yeah, I mean apparently didn't phase them at all. They hear it all.
Jane (36m 23s): Yeah. I was like, I mean I didn't think about it afterwards, but maybe other women that came in like hearing me scream would probably be un unsettling. But you
Sam (36m 31s): Held it together really well. So, you know, I was impressed. I thought I felt really bad. In fact there were a couple of times when I teared up myself because seeing Jane in that much pain was, not to make this about me, but it was hard. Maybe harder on me in a way, but no, it was,
Lisa (36m 50s): You did just say, just kidding. For listeners who might have missed it,
Sam (36m 55s): The men are the real heroes of this. If you, I'm just kidding. Absolutely not. Just kidding. But no for real. But it was tough. Yeah, it was tough to win and all I could really do is I just tried my best to service Jane. Like water, electrolytes, chocolate. She had no appetite though the whole time. Yeah,
Jane (37m 12s): We bought snacks
Sam (37m 12s): But that lasted about six hours. Yeah.
Jane (37m 15s): Yeah.
Sam (37m 15s): Six hours before we got to the, to crescendo to the final act.
Jane (37m 19s): Yeah. I lost my mucus plug and my water broke on the toilet. It was like, I was concerned that I was like, hey, I haven't lost my mucus plug yet. I don't know what I'm gonna go into labor. And then when I saw a mucus plug, I'm like, yeah, that's the mucus plug. And then when I got up I think, I don't know, I just got up to the toilet for one time and then my water burst. It was that big splash.
Sam (37m 42s): Yeah, we all heard the splash, which was interesting. And she was like, I think my water broke. And everyone was like, we all agreed that had had to be that.
Lisa (37m 51s): That's such an ideal.
Sam (37m 52s): Ideal. An hour.
Lisa (37m 53s): Yeah. It was such an ideal place for that to happen, right? Nice and tidy. That’s how my second baby was, yeah. Nice. I was curious about If you had any, wanted to get more specific at all in the ways that you were coping. So I know you, you said you loved or felt it instinctive to be on the toilet, you used nitrous. Were there any vocalizations, were there any other hands-on techniques or any other things that come to mind in terms of how you coped with all of that?
Any, anything that Bori did or Sam did?
Jane (38m 27s): Yeah, I think Bori did some massaging and Sam also did some of that. Like there was some of that counter pressure that was super helpful and music was, I don't know how helpful it was, but I thought in my mind It was like I want music. But yeah, I think just having, honestly just having Sam and Bori there also was just like comforting. I was like, oh, like I was in this different environment and having her there. I think one moment I was like, bore, can you tie my hair? My hair is a mess. Yeah, I think the toilet was just super helpful.
And then I had some, I saw it on Instagram. There were some women that use like a hairbrush in their hands or a comb. Yeah, comb, sorry a comb. Women use a comb to help them. It's like acupuncture with the Yeah, acupressure really. I had, my mom had acupressure, like wooden balls. I was trying, Hmm. So there were almost like stress balls almost. I would've liked to try the comb but they also helped. I like, every time I felt like contraction coming, I would grip on 'em like super tight.
So they were similar. So Sam is similar.
Lisa: So Sam, you didn't get your hand squeezed acupressure? She
Sam (39m 34s): Squeezed my hand. Especially towards the end.
Lisa: She did? Okay.
Sam: Yeah. But it wasn't damaging like people will set me up and be like, she might rip your hand out of your arm socket or something. Nothing like that. It was normal and I was happy to be as helpful as I could be. Mostly again I just tried to make sure she was hydrated. I gave her electrolytes a couple times. Yeah I always offered things. That was pretty much all she wanted though for me.
Jane (39m 60s): Yeah. I tell 'em somebody go away. I was like, just go away. What else was there? I think
Sam (40m 6s): You brought some stuff you didn't end up doing. You were prepared. Oh you had the peanut at one point?
Jane (40m 10s): Oh yeah. I don't remember the peanut like I was like can you gimme the peanut ball? So I would labor on my side or
Sam (40m 16s): Something. You held, you held pillows, like you clutched pillows. Yeah, but all the fancy stuff like get up and walk around the room and do some yoga poses like yeah, that didn't happen that I
Jane (40m 26s): Got annoyed. Met really, really quickly. Early. Early. I was like, no, not happening.
Sam (40m 31s): Smell a candle. No, that wasn't helping. Yeah,
Jane (40m 34s): I think bo set up some like scents as well, but I don't think I smelled it. Like I got the little lights too that you gave us and I bought more of them to dim. But then I was like, I don't even remember like even asking Sam to set it up because I think, 'cause I
Sam (40m 52s): Was, we were past that point.
Jane (40m 52s):. Yeah, we were past that point. Oh sure. I thought about maybe getting into the shower but I was like, oh that toilet's just too comfortable. I don't even wanna walk. Being honest. There was a lot of things that we brought. I think we brought some, like yoga stuff. Like yoga block.
Sam (41m 6s): Yeah, let's say post birth. Having some food that you like to eat was great because like you don't want to eat the hospital food really. Or so we had a lot of snacks and things that were nice to have afterwards. Yeah. And then it, you transitioned to the bed towards the end and there was a few other sort of dramatic things that unfolded before she, she came out right
Jane (41m 26s): On the monitor. I can see the contractions and there was, I had a situation where my contractions were like overlapping and so they cause the, so the contractions were super painful. I think part of it was also that the situation helped me 'cause my labor progressed really quickly because of those like overlapping contractions. But I think that also made it really hard to deal with.
Lisa: Was that maybe transition? Maybe?
Jane: Yeah. I don't remember honestly.
I invited Sam to join this birth story 'cause I feel like he was more lucid than I was.
Lisa: Sure, yeah.
Jane: There were so many things that made sense. I missed that he like caught. So one thing that I'm super grateful that, you know, he spoke up and like even noticed was that the nitrous oxide tank was actually empty. So for a while I was just doing oxygen.
Sam (42m 17s): Yeah. She was humping and puffing it. A
Jane (42m 19s): Placebo effect.
Sam (42m 20s): I know. And I was worried. I was like, man, she has been going to town on this stuff for an hour or two. And I'm like asking the nurse, I'm like, is there any risk of her doing too much of this? And she's, no, if she does too much it'll just fall out of her hand. It's no big deal. And I'm like, that ain't falling out. And I went and I looked and like the little gauge for the nitrous side was at zero. And so I was like, okay, we need to swap this out. And so you were just Yeah, pure placeboing it for at least an hour or two. Just getting pure oxygen. Yeah.
But so you went to the bed and so you did start on your back like normal, like they typically do, right? Yeah.
Jane (42m 56s): I think I was used to sitting on the toilet. My body, I just didn't like moving my body. Like we had a yoga mat and I was trying to do stuff with the yoga mat and I was like, no, this sucks. I can't, this I'm, I'm not digging it. So I went back to the toilet. But then eventually we transitioned to the bed and I just, I know that labor in the back isn't the optimal position sometimes, even though that's how we usually see it in the hospital. So I was on the bed for a bit and then And
Sam (43m 22s): Your contractions were really strong and coming on top of each other? Yeah, yeah. That's what the nurses were saying.
Jane (43m 27s): Yeah. Yeah. And then, and I started making pushing noises when I was on the toilet and bore noticed that and she was like, okay, I remember from your class you have the feeling of the urge to bear down. And I think I was like, I felt that when I was still in the toilet. And then bore was like, notice me, I told Boi that and then she was like, oh, she also heard me making those pushing noises. It was so weird. Like a little grunt. Yeah, it was just like we talked about like your body knows what to do. And I didn't, it just naturally transitioned into those like pushing noises, like without me even thinking about it.
Like it was so strange. It was very instinctual. And so at that point when we were ready to push Bo and Sam notified the midwives and she came in and checked me out and to see if I was ready. So then I started pushing on the, when I was on my back on the bed that then it became all blurry. Then it felt really like fever dream ish. And that's why I was like, Sam probably remembers more of this than I do. I, they stopped giving me the nitrous because like when you're pushing it's not as helpful.
And then, yeah, I just remember screaming at that point. Like
Sam (44m 36s): You were using the nitrous a little bit at first, but I think they were like, after a while they wanted to see more progress. So they had you stop the nitrous to make sure that you could put your full effort behind the pushing. But you did really well. I was like holding your hand and you would, it would come in waves of course and the midwife would be like, okay for this next one, push, push and just back and forth there. The one scary part of all this was the heartbeat, the fetal heartbeat at a certain point, like from all the hard contractions and pushing, it was falling quite a bit.
And her contractions were coming so quickly that it wasn't giving her heartbeat a chance to rebound. And so they were getting concerned towards the end that in fact this was the one intervention that came up as the doctor came in and talked to us about suction because they were concerned that if they didn't get enough progress that it would put the baby's life at risk. 'cause her heartbeat would be just too, she would basically just be crushed for too long trying to get pushed out.
And so the suction as is, is a suction cup put on the crown of her head and then helped to pull her out. We didn't wanna do that. I will say, I asked the doctor, I was like, are there any risks? And she was like, yeah, maybe a little bit, but not really. I was like, I don't know. This whole idea of suction cupping a baby's head. This doesn't sound like the most safe thing in the world. It's like the lesser of two evils. But so what we,
Lisa (46m 11s): And it can be more risky for the mom or parents, a pelvic floor just from the tugging that can cause some damage to the pelvic floor. Interesting. But it can be a way to avoid a cesare in in many cases too. So there's that.
Sam (46m 23s): Yeah, sure. And then we, what ended up making the difference? We didn't agree to that at first. And so what did we do?
Jane (46m 30s): So I think one of the doctors recommended changing positions and so I turned over and went into a kneeling position. And so that I think was really helpful in terms of ultimately getting the baby out and not needing that intervention. But there was also a part of it that like they were telling me not to push. Do you remember that as like we were trying to hold our
Sam (46m 56s): Contractions? So, basically what ended up making the intervention not needed was that Jane needed to skip some contractions basically. So for
Jane (47m 4s): Skip pushing
Sam (47m 5s): During the contractions? Yeah. So for a couple of contractions they said don't push on this one. And so Jane just had to like let it ride. And that was like one of the more memorable parts of this to me was like Jane was grabbing my hand and she was like looking at me and she was like, oh my god, it's great. Like her pupils were as big as dinner plates. She looked like she was on drugs is what it looked like. And she was like, like Sam, that's it. Like looking at me.
Jane (47m 32s): I tried to focus on him
Sam (47m 32s): like just focusing on just intense eye contact and, and as the contractions went through her like a wave and then Audrey's heartbeat bounced back up and so they felt okay continuing. And then ultimately we got you on your knees. Like we flipped her around and that's for where she stayed and where she delivered. And everything went super smoothly after that. Yeah, I say super smoothly. It was still, it was labor. It was,
Jane (47m 55s): Yeah, sure. But I think there was a moment where I was like pushing and I was like, oh, this is the one. And I was like, oh, did I deliver? And they were like, no, you'll know when you deliver.
Sam (48m 5s): Oh yeah, there was a point. Oh man, I felt so bad. There was a point where like she pushed, she pushed super hard, right? And then afterwards, like she asked me like a couple, like a minute later she was like, how is she? And I thought she meant like how is her heartbeat and stuff? I was like, yeah, she's good. And then I realized, oh wait, she thinks she just gave birth. She's about to be very disappointed. I was like, Jane, I hate to break this to you. The baby is still in.
Jane (48m 34s): I know midwives are like, yeah, you'll know
Sam (48m 36s): You're, you are not done yet. You will
Jane (48m 37s): Know. And I had this psychedelic moment too where I was like, I don't know, it was just a lot of hormones and emotions and screaming and it was very confusing. But yeah, ultimately we continued pushing and yeah. And the baby
Sam (48m 58s): Came out. I watched her come out. I wasn't sure if Bob was gonna watch or not. I was like, maybe it's too intense. I don't wanna see that. But by the time it came, I was relieved. I was in it. I was like, yes. It's so satisfying to watch this baby come out and very surreal. It's wild. And then I cut the umbilical cord. Yeah. And then you got her,
Jane (49m 20s): Oh wait. And we talked, forgot about the baby’s first poop, but she actually pooped on me. Oh, fun time. Oh, when she, when she came out, like we had a, you know, we followed your like hospital checklist of breaking our own pillows with like brightly colored pillowcases. She pooped on one of the pillowcases immediately. Oh no. And we're like, let's just go throw that out right now. We don't need that pillowcase anymore.
Sam (49m 44s): Yeah. I think we, we were really happy. We didn't end up doing, I say we, Jane didn't end up doing the epidural because she came out like eyes open looking around and she was just very super alert for hours after birth. Not at all what I expected a newborn to be. It was listless and sleepy. And I think Bori the doula suggested that that's probably to do with skipping the epidural. That's
Jane (50m 10s): One. Oh absolutely. Yeah. I love, that's
Sam (50m 12s): So cool. And you cried and you held her. You were so Yeah,
Jane (50m 15s): It was, she looked like an alien when she first came out. Her head was like cone shaped because of being squeezed and it was so rewarding. After all of that. I felt like the pain just went away instantly. I did have a second degree tear, but at that point I didn't feel anything like, it was just like, oh my God, that's over. We have a healthy baby. Like we didn't have to do the suction cup or the vacuum.
Sam (50m 39s): The one thing that happened was they said the cord was already white when she came out. So like we were gonna wait for the cord to stop pulsating. But that happened almost immediately. So we cut the cord and then they were a little bit concerned that maybe she didn't get oxygen from the cord during some period of the birthing process. So they did some tests, I don't know what it is, but like gas tests basically. And it turned out to be fine. Everything turned out to be a good, good, healthy baby.
She was six pounds and six ounces. Six
Jane (51m 12s): Pounds at 6.5.
Sam (51m 13s): 6.5 pounds. Yeah. And yeah, you had a lot of blood on those sheets. It was wild. I had blood on my shoe. It was like a nice crime scene in there.
Jane (51m 23s): How that happened. Did you keep the shoes? He wiped them.
Sam (51m 28s): Yeah. I probably should say size them, but It was like, it
Jane (51m 31s): Was just like the side of it. It wasn't like on the shoe but yeah, It was like a messy scene afterwards. But they cleaned her up like she was on me and we did like skin to skin immediately. And then we started breastfeeding. The nurse there was super helpful. Like initially I thought there would be more challenges with breastfeeding, but at least for that one, that first time it was very simple. And when they were doing her measurements and everything, they saw that she spit up a little bit of colostrum. And so we're like, okay. She definitely got the colostrum and
Sam (52m 2s): Yeah. More you'll talk more about breastfeeding 'cause that has been a
Jane (52m 4s): Journey for you as well. Yeah. That has been a journey as well.
Sam (52m 7s): But afterwards we went back to the, we recovered
Jane (52m 10s): In the postpartum, the post
Sam (52m 11s): Area in the, yeah. And that was, I was intense. We didn't sleep at all for a long time. I was very out of it. Yeah.
Jane (52m 19s): So are you I think, I think I had like adrenaline or something like just from all the pushing you get a second wind. Yeah. Yeah. And I felt like even though I didn't sleep, I was awake and alert.
Sam (52m 28s): They did. Despite our birth plan, they did want to do certain things that we didn't want 'em to do. Like the erythromycin eye stuff. But they didn't really push it. They were fine. They just explained why they prefer to do it and I explained why I prefer not and it was totally fine. I think that's a big plus for metropolitan. They don't just, they don't not care, but they don't try to push you towards things that you make pretty clear to them you, you want, which is
Jane (52m 56s): Nice. Yeah, they definitely respect the parents' wishes. Nice. So that was really nice. And then we transitioned to the postpartum room and then we were still all a blur. I think breastfeeding got challenging because we didn't have the, It was like we were delivered on the weekend and it was also a holiday weekend. They didn't have their IBCLC there. And so a lot of the nurses were trained in breastfeeding. But you can tell that some were better than others. We were still figuring it out. And then actually Sam was super helpful because he could see the position of the baby when we did get a good latch. And he helped guide me because I was just like, I don't remember what happened.
I was still recovering from the birth. And so he was really helpful there and helping me position the baby. That's how we got a good latch. And
Sam (53m 42s): It was hard though, like we were both exhausted, like super exhausted.
Jane (53m 47s): She was also so tiny. And then we like, we are not really familiar with holding a baby. And so we were like ah, every time we held her we're nervous. It was annoying to have the nurses come in and do checkups every once in a while. But it was also on the flip side really good that they were there because we could ask questions. There was a case where she had some gas that she was crying and we were like, what's happening? And so they helped alleviate that
Sam (54m 12s): Gas. But it was interesting, even though that's true, like they all nurses, a lot of, they still had different opinions on things on the best way to hold the baby, the best way to wrap the baby. Like they, they don't have a lot of this stuff standardized to the degree that I thought they did.
Lisa (54m 26s): Yeah. And it just drives home the fact that there's almost no one right way to do almost anything in parenting. There's a lot of different options but it, but that can be that much more overwhelming or confusing when you've never done this before. And often as we're shifting from this, having been someone's child and being told what to do for much of our lives and shifting into the parental chair of, okay, now you are the one that's making the, making those calls, it takes some time to get used to that instead of, most of us when we're becoming parents who are like, just tell me what to do.
Tell me what to do. And yet now we're, we're the ones parenting and, and we're making those decisions on our own that can take a little while to adjust to.
Jane (55m 12s): Yeah. Yeah. I think we're also like, just can't believe like we're parents now at that point we were like, oh my god, like we're we produce this like little human being.
Sam (55m 22s): You did say that stereotypical thing like that, that during the labor, like when it was really rough, you did look at me and you're like, why did we do this?
Jane (55m 31s): I did. Why are
Lisa (55m 32s): We almost everybody has a moment like that or
Jane (55m 34s): More than I was like when I'm in a tough situation, I go, I think about what are all the things I did that caused me to end up in this situation. And so I felt that and I was like, oh my god. Like why am I here? There was a moment where I'm like, I'm very happy that we did the birth unmedicated, but then there was a moment where I'm like, maybe I should have gotten the epidural at, at that point It was too late. There is like an optimal window where you can get the epidural. But for me I was like, okay, I'm in this. But at the same time I did have the thoughts of like, what if there was a different path that was less painful.
But I think seeing her still alert a transition. Yeah. Seeing her so alert and just curious in the first hours of life was just so worth it to me. She was like, her eyes were looking around the room. Her, she was kicking, she was swaddled and so the swaddle, it looked like a little tail. She was like wagging her little tail. But yeah, it was just so, such a great experience that I'm like, oh I definitely, you know, it was tough and there's so many things in life that are tough, but that it was just so worth it.
And I remember thinking back to your class, you're like, oh, like L labor is like pain with purpose, right? It was like, okay, there's a purpose behind this. It's not just me like suffering but seeing it at the end. It was really worth it.
Sam (56m 52s): She came out super cute. She's the cutest newborn I've seen. I know I'm biased, but she really didn't. She
Jane (56m 57s): Didn't,
Lisa (56m 57s): Not at all.
Sam (56m 58s): I think part of it too might be that she was a week late. Right? She, she wasn't like, she was maybe more fully formed, but she didn't come out all scrunched up and bizarre looking. She was a little smooshed, but she inflated pretty quickly. And we were out of that hospital within like the next day. We didn't stay there. They did suggest that we stay there an additional day and we said we don't really see a need to do that. So we got out of there after the 24 hour period. We were probably only there a total of what? Like 20. See we got, so we got there like midnight that Saturday and then we, when were we, were we back home Monday morning?
Jane (57m 31s): Yeah, Monday afternoon. That's where we left the hospital. I think we were also just tired of the hospital food because it was Oh man, no salt. Yeah, no salt. Salt in food. And they were like, it's no salt. Yeah. It was not the best food. That was like not the highlight of the experience. But
Sam (57m 47s): You don't go to the hospital for the food. Yeah.
Jane (57m 50s): But I thought the whole hospital there was like a sofa for Sam to sleep on.
Sam (57m 55s): It was nice. It folded out and so I could actually put my feet up and sleep. Like I know that's selfish but I When you've been without sleep for like a solid day, like you really want It's nice. Yeah. Anything. Yeah. Yeah. Yeah.
Jane (58m 6s): And the bathroom was like, there was a shower. I didn't, I was concerned about showering. This sounds gross, but I took a few days to be okay. To shower because there were so many things just happened. Sure. And I was bleeding and I was just like, okay, I'm just gonna wipe myself a little and then wait until I feel like I'm ready.
Lisa (58m 24s): So you came home and you had a home visit pretty soon after from a friend of mine who's a
Jane (58m 30s): Lactation consultant. Yes. Kara was the person I spoke to at that time and she gave me a lot of good advice about breastfeeding. I did your natural breastfeeding course and like I, I did that before going to her and then I had a lot of questions and she actually answered all of them. I think the most helpful thing is like I had a list of things I was gonna buy and then she was like, oh honestly, like you can hold off on that. Like those, you don't really need it right away. And plus we live in the age of Amazon, so like Right. You can literally order it and get it next day.
That was good. I had a bunch of questions that she helped answer. So that was, and then she was like, when the baby comes text us and then we can schedule a home visit and to make sure that you're set up for breastfeeding. So I texted Celia lactation when I was in the hospital so I was like, Hey, I just delivered, when can you come to our place and get a visit set up? And so that was really helpful. I think in the early days we're always thinking like, Hey, are we feeding our baby enough?
We can't really see what we're feeding them. They're like just, they're feeding and they spit up and you're like, okay, they had something. But having Annie come over and she did the measurement. So she'll measure the baby prior to feeding and then measure the baby on the scale. Yeah. And then, yeah, it's a meticulous scale. Yeah, it was crazy. It was really good. And it made us, it made me feel good that she was like, oh actually Audrey's like a great feeder. Like she gained this much after feeding. And so that was really helpful. I actually had some like nipple damage as well when I was at the hospital, which was because there were so many nurses and I think some of the latches weren't optimal.
And so I had some pain and I had a crack nipple, which I'm still dealing with right now. But that has improved. Initially I was looking at Sam, I'm like, oh my God, do you think this is ever gonna heal? Like, I don't know. And but, And he assured me that it was fine. The pediatrician assured me it was fine. It was just like an interesting injury because it's like, it, there was like a fissure right. And I was concerned it won't close because the baby's like feeding all the time. Right. And then she also has a habit of cluster feeding.
And so I feel like the nipple was constantly being chewed on by an infant and I was like, it's never gonna close. This injury's gonna stay open forever. And so I, I read more about it as well online and it's, the injury doesn't just close. It gets less shallow. So it's important to keep it moist, not form a scab. Mm. And so that I think was the hardest part. I think it was just painful for me to breastfeed and I think I had damage on both my nipples but one was a little smaller and one was a little worse.
And I'm grateful to say that they're both mainly healed now. So it's yay. It definitely takes a little time. Definitely. Yeah. It takes some time and I think breastfeeding has definitely gotten easier as well. Like it was great to help Annie's help. I didn't, the thing is there's a lot of stuff around like the parenting industry where you're like, oh I need a breastfeeding pillow and all these like different accessories. Andy's recommendation is like, hey, you don't need a breastfeeding pillow. And so like we with your natural breastfeeding course and Andy's recommendation like we just needed to just get some pillows supported and yeah it was great.
I'm definitely feeling more confident about breastfeeding now. Like since Annie's visit she came another time and we have some virtual appointments set up with her. Yeah. And so it was just really helpful to get that extra support 'cause we didn't get that at the hospital. Right. And breastfeeding, she's going super right now. She was born 6.5 pounds and now she's almost 10 pounds in a month. In a month. Like she was, I was like wow. Clearly feeding. Well she is a hungry baby. There is definitely a lot of cluster feeding in the morning, in the evenings.
I'm very grateful when she does take a long nap. I'm like, okay. My cracked nipple gets a break.
Lisa (1h 2m 29s): Yeah. Oh and with the support that you got with and with the cracked nipple was, was there any like a nipple shield that was recommended to use or just not just keep feeding? No,
Jane (1h 2m 41s): I just keep feeding. Like it was a little painful and I don't think anyone was like, oh yeah, I think they understood like it was painful. But before my ma milk came in, Jaye helped me use the Haakaa too, so I would feed her from my, my good nipple and then have the haka going on my other on the damaged one. And then that gave it a break. So that 24 hour break actually was super helpful. It stopped the bleeding and then we fed her with the syringe from the milk that was like obtained from the haka
Lisa (1h 3m 11s): Hand express. Huh.
Jane (1h 3m 12s): So that was, yeah that was super helpful in terms of getting that initial like break from the damaged nipple, sorry.
Lisa (1h 3m 20s): Oh nice. Yeah. And with the Haakaa, was it just that from the letdown reflux you were just leaking while you were feeding on the other side? Or were you actually like pumping
Jane (1h 3m 29s): With that? Yeah, that suction, yeah, the manual one definitely bugs me. Yeah.
Lisa (1h 3m 34s): Cool. Yeah. So yeah, I'm glad that's healing and I'm glad you've had some good support on that.
Jane (1h 3m 39s): Yeah.
Sam (1h 3m 40s): And you were, this is another example of Jane thinking that nothing's gonna improve. She was very upset about her crack noble for a while. And like the lactation consultant, the doula, the pediatrician, everyone's, it's okay, it's going to heal. It's not that bad. It
Jane (1h 3m 54s): Just looked
Sam (1h 3m 55s): Really bad and she was just convinced it's never gonna heal. And then now like yesterday she looked so happy she said Look, it's healing. Yeah, wow. Just as everyone on earth has assured you. So
Lisa (1h 4m 5s): I think she's on her own timeframe with that. Yeah,
Sam (1h 4m 8s): It's fine. It's good. Like I'm, it's good that she's, I like how conscientious Jane is and she's really impressed me from start to finish. She really blew my mind during the labor. That was an act of extraordinary strength and she's really done super well with Audrey since then. And I feel like I married really well.
Jane (1h 4m 26s): Aw, thanks. Aww. I think breastfeeding was just really hard initially. That was definitely something like getting the positioning right and sometimes she's fussing and I have like nipple pain and that, I think that part was just really hard. I feel like now a month in we, we both got better at breastfeeding. So I think it's definitely better. I think postpartum overall the physical recovery hasn't been super challenging. I think mostly it was just emotional. I did have some baby blues where there was a, like you have just a lot of emotions.
Like part of It was like, oh my God, she's not gonna be this small forever. That kind of, I think that Google, It was like anticipated nostalgia and the thing of the babies, like they're always changing and they're always growing. Like she looks so different than she did a month ago and I'm like, oh I'm never gonna get those days back. All those like,
Lisa (1h 5m 15s): It's a very bittersweet,
Jane (1h 5m 17s): Yeah, it was crazy complicated. And then there's the sleeplessness where you're like, oh my God, I'm so tired. Am I ever gonna sleep again? And then sometimes also the part I feel worse about is sometimes I feel like when I'm sleep deprived I'm not my best self and I'm like, oh I should really be, just be more patient with her. She's just a baby. And sometimes I'm like, oh, why don't she just sleep like it? It is just hard. I feel that guilt of oh I need to be present, but at the same time I'm sleep deprived myself and I can't give her the best of me.
And so that's been hard as well. So yeah, there's just a lot of emotions and even like when Sam was around I'm like, oh I miss you. I felt like we didn't get a lot of time 'cause we were all like focused on the baby and so there was just a lot of mixed emotions around it for sure. Sure.
Lisa (1h 6m 6s): Yeah. It's so multi-layered for sure. And Sam, any reflections for you in terms of what it's been like transitioning into becoming a parent?
Jane (1h 6m 18s): Lemme
Sam (1h 6m 18s): Push that mic. I think it has been overwhelmingly positive. I love my little baby. She's so cute and I love her and she's so funny and interesting and I'm enjoying watching her develop her abilities. I do wish in hindsight I'd taken more paternity leave. Like when you're in sales and you work heavily on commission. Yeah, I could take time off and like my employers were willing to give me a few months off, but like they can't pay me commission on deals. I don't close. Right. So, ah, yeah, it would be a pretty big hit.
So I took a few weeks, but in hindsight I wish really I just sucked it up and just took the monetary hit and gone ahead and, and basically maxed out my pat leave. So that's a lesson learned and not because like I'm, I work from home so I still get plenty of time with the baby really, but more to help Jane out with her during the day. But whatever, live and learn, if that's the worst thing that I've done then I think I came out pretty good here. And I don't know, I'm very happy. I'm very, I love seeing Jane be a mommy.
She does such a good job and she's doing a great job as evidenced by how fat her baby is.
Jane (1h 7m 27s): And, and
Sam (1h 7m 28s): I'm just, I'm super stoked. I feel very lucky. I feel very grateful that Audrey knock on wood so far has been very healthy. And as a parent, I think that's all you really want.
Jane (1h 7m 39s): Funniest facial expression. So she's always very curious and furring her brows. Yeah, it's cute.
Sam (1h 7m 46s): She's, and she's finally getting to where she can see better, so she's like looking at our faces more. Mm. She's like looking at shapes. We have those black and white cards and we're, we're doing everything we can to set her up for success.
Lisa (1h 7m 60s): Nice. Wonderful. Is there anything, as we start to wind things down, is there anything that you didn't get to share that you'd like to share? And if not, any final words of advice or reflections for folks who are listening, many of whom are expecting a baby?
Jane (1h 8m 19s): I think you had one, you were like, I think so. I definitely like to be prepared, like prior to giving birth and everything, I was like, not only thinking about some of the health aspects of it or like delivery and stuff like that. We also prepared like college savings, estate planning, all that stuff. And I think initially Sam was like, he didn't know I, I was more familiar with doulas and lactation consultants because of my like background of having worked in like that industry before.
But I think Sam was like, oh man, I'm really glad that we ended up using those resources because like you can say it.
Sam (1h 8m 58s): Yeah, I would say, I think at first I was like, I don't know Jane, you're a bit of a nerd. Okay. Like we've been having babies for a million years in caves, like we're gonna be fine. But in hindsight, yeah, like she took advantage of every resource she could that her employer gave her, that the hospital gave her programs like yours. And I thought it was way overkill at first. And in hindsight I think all of it helped and it made the birthing process a lot more, I guess a lot less harrowing.
It gave us a lot more confidence. I will say one thing, and this isn't like a ding against metropolitan specifically just the healthcare industry in general. If you show up unprepared, they're, you are just gonna, they're gonna take you wherever they want to take you. And it might be for good reasons and it might be for less good reasons. It might be aligned with your values and it might not be. So I feel bad for people who show up and just expect that whatever medical professional or organization is just gonna have the best in mind for them and it's just gonna give them the best treatment in all cases.
Even if they show up completely uneducated and uninformed. It's just not the case. I think a lot of people, because we showed up maximally informed and there were still times where we were not pressured. But had we not, if we had even slightly less resolve, if we had even slightly less resolve and had been slightly less informed, I think we would've agreed to some things or made some decisions that we would be regretting right now.
So I guess the best way to prevent regrets is to just maximally inform yourself, show up at a plan. And we did that. I'm rambling I guess I'll say. No, you're not.
Lisa (1h 10m 52s): You cut out. I love it. It's
Sam (1h 10m 54s): Great. I'll just put a, I'll put a bow on it and I'll say like, just take advantage of every resource you can. You don't have to be obsessive about it, but none of your time spent learning about the birthing process is going to be wasted.
Lisa (1h 11m 12s): Yeah. Thank you so much. That's wise words. Yeah. It's unfortunate that we live in a society, in a culture, in a country in which we really need to prepare and equip ourselves and be our own best advocates. But in the maternal healthcare field in particular, it is. It's just the current state of things. Yeah, just listen to Sam, thank you so much. What an honor and a pleasure to reconnect with you and to get to see Little Audrey.
She's so adorable. So I really appreciate you taking the time, especially in these early weeks of being a new parent and being exhausted. I know you have a lot going on, so I just really appreciate it a lot.
Jane (1h 11m 58s): Thanks for having us. I think, you know, her birth is really special and I think we wanted to join you because we also wanna record like and remember that moment because that moment is just, I barely remember it now. So it was nice to be able to reflect on that and be able to remember it.
Lisa (1h 12m 19s): It's still fresh and in particular. Yeah, as fresh as it can be given you were in labor land. Wonderful. Thanks again.
Jane (1h 12m 27s): Thank you. Bye
Speaker 6 (1h 12m 28s): Bye. Bye.
Lisa (1h 12m 29s): Alright, so that was Jane's and Sam's story. I'm about to leave on a short vacation with the family tomorrow, last hurrah for the summer. So I'm not gonna do any extra teaching here at the end, but I will give you a quick teaser of what's up next time as well as Jane's mantra in labor. So here's the teaser.
Eric (1h 12m 49s): I'm a skeptical person. I'm skeptical of everything. So some of the advice I was like, I don't, this seems a little silly, this seems a little crunchy granola as you said. And I was pretty surprised we took a, A lot of the advice you gave was really helpful. It was like hindsight. Yeah. Yeah. I was just like, wow, we really use, if we hadn't taken that class, not the doctors and nurses just tell you stuff and you're like, okay, I guess I gotta do this 'cause you don't know. But I asked, both of us asked a lot of questions or said, I think, is this medically necessary? What is the end goal here?
What is the point of doing these specific things? And they would say a lot of 'em would be confused. They, it would be like nobody ever asked them
Anastasiya (1h 13m 26s): Before. Yes, yes. A lot of, you know,
Eric (1h 13m 27s): They're like, oh, I never got that question before. Yes. So they're, I guess you can wait. You know, it was very helpful actually.
Anastasiya (1h 13m 33s): That was the big, I think the biggest was yes, as Eric said, realizing that you can always ask questions and that it's your body.
Lisa (1h 13m 43s): All right. So that's your sneak peek for the next episode. And then Jane shared with me her favorite mantra for labor, which is the phrase, pain with a positive purpose. If you've taken or will take birth class with me, you'll be familiar with this phrase, the fact that birth is a natural, normal, biological process and the intense physical sensations we feel are purposeful and are a positive feedback loop. There's a baby at the end of this. There's a baby at the end of this.
So I'll encourage you to sit with this idea of pain with a positive purpose or If you prefer the wording intensity with a positive purpose, take advantage of the concept of neural plasticity or our ability to change the ways our brains are thinking about things and rewrite the script in your brain with repetition and consistent reinforcement of this idea. Thanks so much for listening to the Birth Matters podcast. If you like this podcast, won't you please share it with a friend, leave a review where you can, and of course be sure you're subscribed or following so you don't miss any new episodes.
Have a wonderful rest of your summer and we'll see you next time.