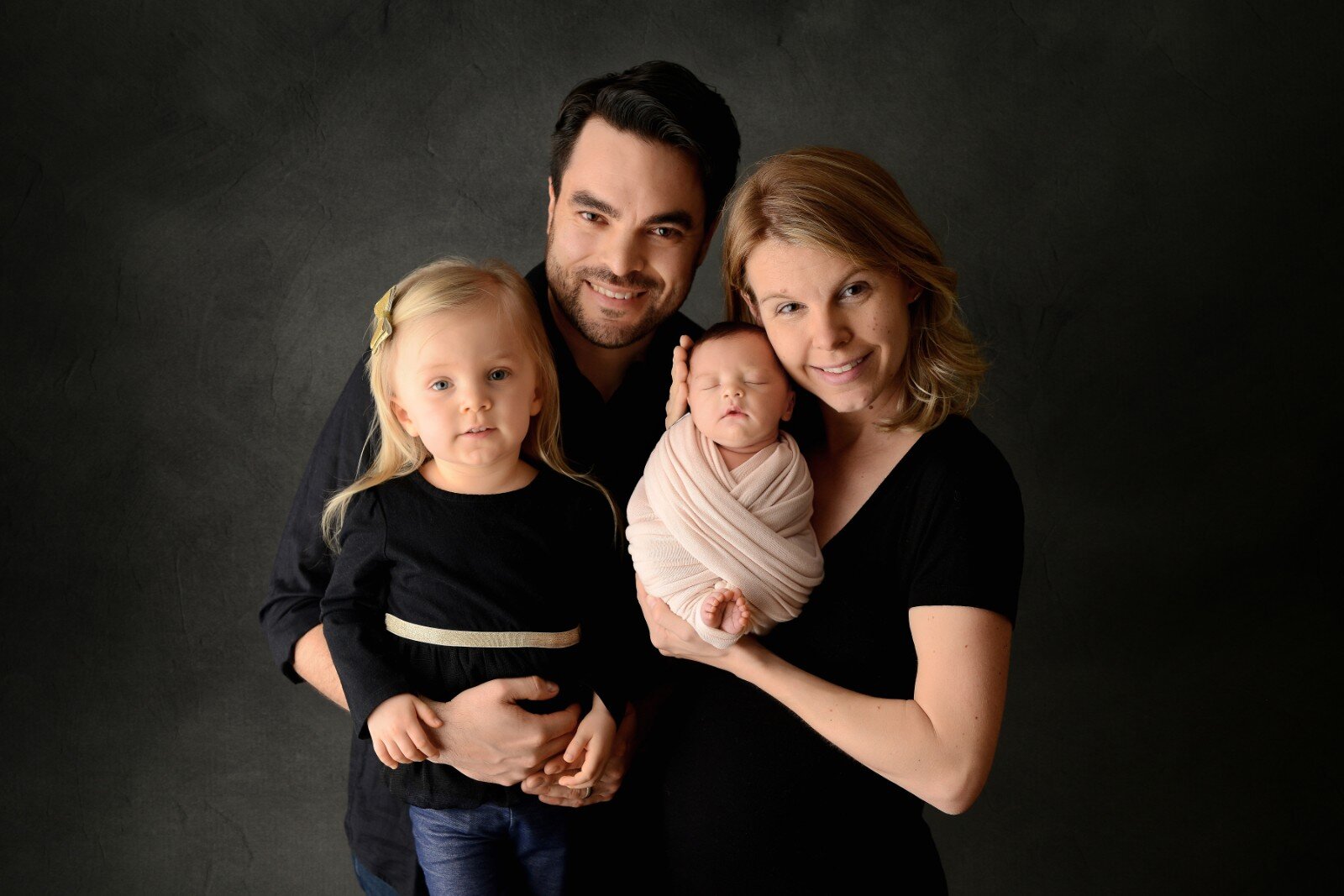
Today you get a 2-for-1 -- 2 birth stories from one mama. Melissa has an almost 3-year-old, Segovia, and a 6-week old, Adelina. She shares her first 1st birth story, which was an unusually quick, 6-hour induction with no pain meds and with doula support. Then she shares her rationale for switching care providers from an OB over to working with a hospital midwife for her 2nd baby’s birth, which was an even faster, 4-hour, unmedicated labor.
Episode Topics:
1st Pregnancy/Birth Story
cholestasis led to induction 5 days before due date
checking into hospital for cervidil (cervical ripener), avoiding epidural due to chiari malformation (a condition in which brain tissue extends into your spinal canal)
description of what her contractions beginning felt like, doula (Dawn Chorba) joining them
resident saying they’re about to start pitocin; Dawn encourages them to advocate for themselves, which leads to declining pitocin as Melissa preferred
Melissa loving homemade switchel (“laborade”) as her healthy labor electrolyte drink
mini-goals as a helpful strategic tool
identifying the baby’s sex
grateful for doula taking photos, skin to skin/immediate bonding time and joy, asking for them to not wash off the vernix and delay the bath
the decision to switch care providers from one birth to the next (OB to midwife Melanie Summersille at NYU Winthrop on Long Island)
talking about her decision to have children after not being sure that she’d ever get married or have children, having come from divorced parents and moving far away from family support
2nd Pregnancy/Birth Story
conceiving 2nd time after only a couple months of trying
harder pregnancy; spontaneous labor begins (no cholestasis, no induction) and is done in only 4 hours, GBS positive but no time for antibiotics
pushing stage, giving birth in bed on knees, leaning over a peanut ball
difference in midwifery care (hint: she highly recommends it and wishes it had been on her radar the first time around)
postpartum / breastfeeding reflections
tip for parents giving birth for the 2nd time - make it a priority to get 1-on-1 time with each child
Resources:
Intrahepatic cholestasis of pregnancy - reduction or stoppage of bile flow, 1 in 1,000 pregnancies
Switchel recipe (Wellness Mama)
**Disclosure: Links on this page to products are affiliate links; I will receive a small commission on any products you purchase at no additional cost to you.**
Transcript:
Lisa: 0:00
You are listening to the Birth Matters Podcast, episode 15.
Melissa: 0:04
I just remember thinking like through each contraction, like, "You can do anything for 60 minutes, you can do anything"–or, 60 minutes, "for 60 seconds, you can do anything for 90 seconds," you know, however long it was lasting. I was like, I was like, I can do this, I can do this." Then like, just almost like the little engine that could. I was like, "I can, I can, I can'." Like, and it really helped to kind of focus on that like it was just a short period of time.
Lisa: 0:38
Hey, there. And welcome to the Birth Matters Show. I'm your host, Lisa Greaves Taylor, founder of Birth Matters NYC Childbirth Education and Labor Support. This show is here to lessen your overwhelm on the journey into parenthood by equipping and encouraging you with current best evidence info and soulful interviews with parents and birth pros. Please keep in mind the information on the show is not intended as medical advice, or to diagnose or treat any medical conditions. Have you subscribed to the show yet? Please be sure to do that wherever you're listening to this or over at birthmattersshow.com so you don't miss out on anything.
Today you get a two for one. Two birth stories from one mama. Melissa has an almost three year old, Segovia, and a six week old, Adelina. She shares her first birth story, which was an unusually quick six-hour induction with no pain meds and with doula support. Then she shares her rationale for switching care providers from an OB over to working with a hospital midwife for her second baby's birth, which was an even faster four-hour unmedicated labor. I wanted to mention that we had some technical issues with the audio for this episode. You'll hear an echo on my voice at times, but we edited out or replaced most of my talking and re-recorded the things we needed to so that it would be more or less knowable. We couldn't fix the audio problems and clicking sounds that occurred with Melissa's voice, but I really wanted you to hear Melissa's stories.
Before we get started on the birth story, today's episode is brought to you by the Birth Matters Complete Online Course. If you can't squeeze in an in person group birth class series or if you didn't feel like the one you took was comprehensive enough, or if you don't even have a quality class available in your area, I have the perfect solution for you: Birth Matters Complete Course is an online recorded version of my in-person full series. It covers not only prep for an amazing birth with self-advocacy tips, best current evidence and tips for partners, but also holistic postpartum wellness, breastfeeding and newborn care. And to top it off, you get lifetime access so that you can use it as a refresher later in this or future pregnancies. Check it out at birthmattersonline.com. Now let's get started with today's birth story.
Melissa: 2:53
My name is Melissa and I am just, you know, taking care of my second little one who was born almost six weeks ago. I have one daughter already, her name is Segovia, who is about to turn three in a week. So we're really looking forward to that. And yeah, it's been challenging, but also very incredible, all the same. So my parenting journey is going, I think it's smooth and as good as one could hope so far. I mean there's always challenges, but right now things are, are pretty good, so I'm happy about it. So I've had two birth experiences, one obviously with my three year old and then the one with little Adelina here who was just born. I found the second one, the birthing experience to be easier, ironically. But the first one there was definitely, you know, some anxiety about giving birth and what to do and how it was going to happen and all of that. So with my first birth, I decided to use a doula because I just thought somebody who's been through the experience and has techniques that can help me would be a really, really helpful tool.
So we used a woman named Dawn Chorba, and she is fantastic. She has two kids of her own now and hasn't gone back to doula-ing just yet, because of her second baby, but plans to, and is running some support groups for, for new moms and old moms alike. So she was super helpful, as was your Birth Matters class. There definitely were things that I took into the birth just from memory and from reading up, you know, after the class, that like really helped me get through the process because it can be scary because you never experienced it before and like, you know, your body's doing all these crazy things to try and bring this tiny human into the world, and it just really helps to have people who, you know, knew what they were talking about. That helped me through the first round. Definitely. And a lot of it stuck with me even for the second one. And so that was really useful.
With the first one, I wound up in my third trimester having cholestasis. So, my OB-GYN at the time kept pushing back like the time that she wanted to induce me because my levels– for people who don't know, cholestasis is when your liver bile levels abate, and it can cause complications for the baby during birth. So if they get too high, the doctors will recommend being induced earlier than your due date. So I was nervous about that. I didn't really want to be induced. I was hoping to kind of have more of just like that natural, you know, it takes shape on its own type of experience, but you know, that wasn't the destiny for the first baby. So I was only induced about five days early, which is pretty good for somebody with that condition. So when I went in to the hospital, they told me at first that I was going to be given Cytotec, which is a cervix ripener where they literally insert like a little pill–they call it a tic tac, in, you know, up near the cervix so that it ripens and you're ready for birth. They recommended that I do that three times. And after that they told me I was going to start to get Pitocin, which after all the readings and for class and all of these things, like I was really, really nervous about getting Pitocin,and I didn't want it at all.
So prior to the induction I was very anxious and like, you know, had a few bouts of crying and I was just fearful that it was just going to make it not as natural as I wanted it to be. On top of that, I was very determined not to have an epidural, just for multiple reasons from stories that my friends told me about, just like things that have gone wrong with their epidurals, back pains. And then I also have what's called a chiari malformation, which is a nervous system issue. And I didn't want to even take 0.005% chance that it could mess with that. So because there would insert–they insert a needle into your spinal cord, which I was like, "Ah, no, I don't think that's a good idea for somebody with my underlying issue."
So I did state to the hospital, to the nurses, and my doctor that I didn't want an epidural. So definitely having Dawn there helped me get through that because it's painful to go through all of the contractions, but. So when I was in the hospital, they gave me one round of the Cytotec, which they make you lay flat on your back for an hour and then they let you get up to go to the bathroom and walk around for like two minutes and then they let make you lay back down to start it again. They don't want it to move or shift, it's just like a little pill. So you have to basically just lie flat on your back and just stare at the ceiling essentially. Also, I was hooked up to like, you know, the contraction monitors and I did have an IV, so that was slightly uncomfortable. I did do the second round of the Cytotec, and midway through the hour, I felt like I had to go to the bathroom. I felt like I needed to have a bowel movement. So, and I was begging the nurses, "Please let me get up, please let me get up, let me get up." And they were just like, "No, you need to stay laying down. You just go laying down. If you need to go, we'll bring you a bedpan." I was like, "No way." So I just held it in for like as long as possible and they let me go finally.
But after that I still felt like I really had to go to the bathroom and I was like, "This is really uncomfortable. Like, how can I still have to go?" But then the monitor was showing that my contractions had started actually. And so they were picking up and it wasn't actually me having to go to the bathroom. It was that I was in labor. So at this point, you know, I woke my husband up and I was like, "You need to call Dawn and have her come to the hospital." So he called her and she came to the hospital about four or five minutes later and I never had to have the third round because I was having contractions. And I was also very lucky that the nurse that was with me at the hospital, she was studying to be a midwife. So that was amazing. Like she was all for a natural birth and she, she kept telling me, she's like, "All the other nurses are so thankful I got you. Because some of them don't like dealing with like natural births, they'd rather just do the epidural." And and I was like, "Wow, that's surprising, actually," because I don't know, I just thought they would be willing to help with all of that. But I guess some of them just prefer like the patients to be a little bit more calm.
So Nurse Jackie, ironically, she was all for it, and actually just like excited that, she's like, "Oh my gosh, you don't want an epidural? Like you want to do this naturally?" And I was like, "Yes, I do." So she was super excited. I think it was kind of helpful for her too and her journey to becoming a midwife that I fell into her lap sort of that night. So she helped me through–unfortunately she went on her dinner break, like, when all the contractions were happening. So I had like a substitute nurse in for an hour during this like crucial time and also my OB-GYN wasn't on call yet, she was coming in the morning thinking that the process was going to take a lot longer. So it was just a resident OB-GYN there and she kept telling me, she's like, "Okay, well we're still going to start the Pitocin for you at like, you know, in like an hour," you know, and I was like, "But I'm having active labor. Like I'm having contractions. Like what do I need the Pitocin for?" She was like, "Yeah, but you know, your chart says this." And I was like, finally, like, when Dawn was there, she's like, "Ask her to leave the room. Let's take a minute, you know, in the short time that like you have in between contractions."
Melissa: 11:31
So we took, you know, a minute or two and she said, "Just ask her to call your doctor and you know, and just advocate for yourself." And so, you know, thankfully she was there because my husband is wonderful, but you know, it's also his first time doing this. So he didn't really know like what to do. And so, so they did call my OB-GYN, and she said, "No, you don't have to have it." And it was just like a complete relief for me because I was like, "This is already painful. I can't imagine like adding Pitocin and making it faster and stronger," you know, in the middle of all of this. So after that, like we just kind of, you know, made it through all of the contractions and they started to get, you know, you know, shorter in between, and longer and stronger and I actually had prepared that that switchel drink that you, that you drink. And we had–Brian kept bringing me, like, fresh bottles of it, cold, and I don't even know how many bottles of it I drank. It must have been, I have no clue. So much so that she had to like, put in a temporary catheter after the birth because I drank so much and I had the IV, that like my bladder was just like full at the end.
So through that process, hard to really remember like the intensity other than I can remember now from the second birth. I just remember thinking like through each contraction, like, "You can do anything for 60 minutes, you can do anything"–or, 60 minutes, "for 60 seconds, you can do anything for 90 seconds," you know, however long it was lasting. I was like, I was like, "I can do this, I can do this." Then like, just almost like the little engine that could. I was like, "I can, I can, I can'." Like, and it really helped to kind of focus on that like it was just a short period of time. Even though time feels very infinite in that in my mind, like that birth from the time I started feeling the contractions to when my daughter was born was only six hours. But yeah, it was really quick. Well, I didn't even have to have Pitocin, so I kind of I think started naturally luckily yet it was crazy. It could have felt that way. It could have been, you know, two days. I had no idea. You know, when you're in that zone, like it could have been five minutes, it could have been, you know, three days. It just, it's just crazy. Time, it doesn't even exist. You're living in like a vortex or something.
So then finally after changing positions several times and I guess I was finally ready to push and finally saw my doctor when she came in and you know, prepared me to push, and you know, the next thing I knew my daughter was here and so we didn't know what sex was for the first baby, for Sigovia. And so we were anxiously awaiting that. And so when she came out and they actually said, "It's a girl!" like they do in the movies, it was really amazing. It was like such a cool feeling and like, you know, like all these emotions just like rush over you and you just forget about all that pain you just went through and it's, it's really insane how it just like stops. Like you're just like, that pain was lasting all this time and then all of a sudden nothing. You're like, "Oh, okay, here we are" and you know, my husband was crying and I was actually really thankful also that Dawn was there because she took pictures and like, you know, that's not something he would be capable of doing the moment. And so we have some, you know, picture reminders of just like that whole experience. So that was really, really amazing.
We decided with her and with Adelina as well, too, you know, to have them keep the vernix on. Like I asked them not to wash them off, or you know, until much later. And most of the hospitals now are letting you do like the skin-to-skin for a long, longer period of time, which is really a good push forward I think. So I kept her on me for, you know, however long they let me and you know, they did take her to measure her and weigh her and all that, but then brought her right back. And, I don't know. I just remember chaos versus like selecting what things and shuffling me along to the next room. But like you just don't even care because you just have this little baby like laying on you that's wasn't, wasn't there before and it's just, it's insane actually. It's just like the craziest, most amazing thing. So yes, that was my, my first birth experience and it was, it was incredible. Hard but incredible.
Lisa: 16:14
And you were out at LIJ?
Melissa: 16:14
The first one I was at North Shore Manhasset, which is now Northwell Health I think. So. And then I switched for my second birth, so I actually went to Minneola to go to the NYU Winthrop. It was where she was born just six weeks ago.
Lisa: 16:35
Can you talk a little bit about what caused you to want to switch care providers?
Melissa: 16:40
Sure. So because of the induction process and the Pitocin, I was told during my followup visit by my OB-GYN at the time, that if it had been my second birth that they would have just gone straight to the Pitocin. And you know, with things like the condition I have, with cholestasis, it's likely that you'll get it a second time, which means that likely that you'll have to be induced again, just by the standards of the medical profession. And so I was not thrilled with that answer when she's like, "Oh yeah, if you have another baby and you have this, like, you'll just get the Pitocin right away." And I was like, "No, no, I won't. Like, I don't want that to happen." And so that was like one thing.
And then in the practice that she was in there, there were three other doctors and one of the doctors who I had seen prior, too, and so was doctor in the hospital the next day after Segovia was born also kind of was telling me that I really couldn't do it without getting an epidural, and that I would change my mind. And I was kind of really turned off by that. Like I just didn't like the fact that he was like, "Oh yeah, most first time moms, they say that and then, and then they wind up getting epidural anyway." And I was like, "But I'm not...like I have a condition that I know it's not good for. And I've heard too many stories from friends and you know, family members who have had issues with the epidural that it's not something that I want. Not saying it doesn't work for some people and probably most people. But for me it's not the route I want to take." And, and even after, when he saw me the next day, when the baby was here, he had told me that, he's like, "Oh, how did it go?" He asked, you know, asked about it. And I was like, "Oh, well I didn't wind up needing the epidural, and he just kind of like shrugged it off, you know, did everything but rolled his eyes basically. And I was like, "Yeah, I think I'm kind of like finished with you guys. Like I don't really like this mentality. So we weren't sure we were going to have a second baby. I wasn't sure I was going to have the first baby.
Lisa: 18:56
Do you want to talk about that at all?
Melissa: 18:56
Sure. Yeah, I think it's something that people don't talk about a lot. I don't know. It's like either you, you do have kids or you don't have kids. And a lot of people aren't comfortable with sharing like why they chose not to or why they couldn't, or, why they chose to have children. And that journey was long for me. Like I definitely...growing up, you know, I came from divorced parents, you know, I moved away from home, like [inaudible] originally and I moved to New York pretty much on my own. You know, I developed a life here. Everything has gone well for me, but you know, when you don't have your family here, it's like not something you think like, "Oh I'm really gearing up to have kids with no help." You know, that's not really something that you think about.
And so I just never thought that I would get married, first of all. And then I met my husband and that changed. And then it took me a long time to come around to like the idea of having kids. So we were married for six years before we even contemplated like, "Oh, let's try and see." And you know, and also I'm a little bit older. I had my first daughter at 36 and I just had her at 39, so not that that's old by today's standards, but you know you can have a baby at 18 so it is kind of...or younger, some people. So it's, it is a little bit older on the spectrum of like, you know, pregnancy. So I just wasn't sure. And we just finally just decided like, you know, we've done a lot of things for us as a couple and career-wise we were pretty set and so sort of just threw caution to the wind and were like, "If it happens it does and if it doesn't it doesn't and I guess we'll deal with it either way, like, as it comes." I had no plans of ever doing IVF or any of that. Like I just was like, "I'm not going to go through all that if it's, you know, it's for me if, if it happens, it does. And you know, obviously that's the way my life was meant to go, but if it doesn't, I'm not going to pressure myself to make it happen." Because you know, my life was full. I thought it was full anyway before children.
So we got, we actually got pregnant pretty quickly. You know when we decided that and then just kind of went full steam ahead and it wound up being the best blessing. But you, I definitely am onboard with women who decide not to for whatever their circumstances, reasons are. I have several friends, you know, are either single or even married and have decided not to have kids. And I think that's, you know, their choice, and what they want for their lives and you know, it actually makes them better aunties as far as I'm concerned. They come on over and see my kids.
But yeah, so that was kind of my journey with having kids, and then deciding to have a second was sort of reliant on my first daughter because you know, part of it is that we were a little bit older of parents and thinking about like, "Okay when Segovia is our age, like we're going to be like in our seventies, which is hard to imagine. But like what happens if something happens to us, like she's not going to have us forever. And not saying that a sibling solves that issue always. But we gotta give her a chance, I guess, so we decided like, "Okay, like she's pretty great. We love her. So hopefully we'll love another one if, if that's what you know in our, our plan here." So again, we kind of were like, all right, if it happens it does and if it doesn't it doesn't. And again, it only took like, you know, I think two months maybe for us to get pregnant. So I consider myself very, very lucky at this age for that to have happened. I mean, I was wary through both pregnancies that like, "Is this really gonna be good for us, is this really what I want?" Like, you know, and there's still some days that are really hard. I'm like, "Did I make the right decision?" Like I love my, my babies, but at the same time it's like, wow, like some things are definitely much easier without kids.
So I think it's just a lifelong balance of finding yourself and being a mom and your career. And you know, all of that just, it takes time to come around to it. And it's not for everybody. And thankfully it is for me. I wasn't sure it was, but it is, you know. It's just so incredible to, to watch them, you know, grow and go through the phases and especially now that, you know, my little one is like telling me jokes and having full on conversation and wants to read books all the time and sing songs and play at the park and all these things that I was like, "Weren't you you just a baby? Like, how did this happen? Like how are you a human now?" Like it's really, really incredible to watch those like stages and, and just see her brain sort of just like transform. Like it feels like overnight almost. But, yeah, so I'm thankful that I was able to give her, you know, a sibling and we'll see how that'll go this time for sure they'll have their ups and downs and you know, it's just a really cool experience and, I'm thankful that I've gone through it twice. I currently don't have plans to go through it another time. I really don't want to be pregnant after 40 and that's coming in very quickly, in December. So I think this might be it for us on the, the natural kids bandwagon. Maybe there is an adoption in our future, but we'll see.
Lisa: 24:59
Great! Well, why don’t you jump into sharing about your second baby’s birth?
Melissa: 25:06
Sure. So with this little one...she's right here. She is sleeping away. This is Adelina. With her, the pregnancy was a lot harder. I mean that could be for multitudes of reasons, probably because I have two and a half year old running around. I also was more nauseous, full time working full time, two and a half year old. Being a wife, maintaining life in general is just more exhausting through the first and second trimesters. And then my third trimester I didn't get cholestasis. Thank goodness. I didn't have to be induced and none of that was even on the table. Very excited about that. And I also went to see a midwife instead of a OB-GYN so that also helped me to get through it a little bit more positively I guess on the natural side of things. And she was very supportive through the whole thing.
And we did want to originally have Dawn be there again for Adelina, but she recently had her own daughter and wasn't doing the doula process at that moment. So we kind of just held off and didn't really look for another doula. And my birth was fast, so, it's likely that I probably, even if I had one, they wouldn't have arrived in time. So it was okay. I'd had the experience of the first one and actually NYU Winthrop has now a volunteer doula program. I didn't get to use them because my birth was so fast. But I have a friend who was there a few months before me and she did. And the experience for her was really good. Just like with the first one, it was just getting through the process and it was a little bit different in the fact that I didn't have to be induced. So with the first one, I knew I was going in this day and she was going to be born within, you know, a day or two and you know, so that was there. With her, I had no clue when it was coming. You know, like you have a due date and like, you know, my midwife was telling me that like, "Oh, you're a few centimeters dilated, you're pretty much like 90% effaced. For like two weeks, she keeps telling me that, she was like, "You can go anytime." So like every day I'm like, "Today? Is it today? When is this happening?" Even to the point where I had an issue a couple of days before she was born where like I thought my water broke because I didn't really know what that felt like other than in the hospital, the process of everything else going on. So it didn't end up being my water breaking.
But you know, I called my midwife, she's like, "Go to the hospital, they'll just check to make sure that you know that you haven't ruptured. And if you have then obviously you're in labor. And if you haven't, then they'll send you home." And so we went and they sent me home. And we went to get ice cream, because my mom was here watching my daughter and I was like, "Oh, we're actually out. Like let's go get ice cream." So we went and got ice cream and then went home. And then two days later I started to have like similar to that feeling I had when I was in the hospital when I'm like, "Oh there's like a cramping in my stomach. Like, do I have to go to the bathroom? Do I not? Like what's going on?" And you know, I was just slowly but not slowly. It started happening like around six in the evening. It got more frequent and longer. And stronger, I'm sorry. And I was like, "Okay, I think this is actually finally happening."
So I called my husband who wasn't here at the time, called the midwife and she's like, "Oh you should get to the hospital because I've been telling you you're going to go quick." And I was like, "Oh you know," like "Everybody says it takes longer." I mean I thought I would go fast because Sokovia was six hours. But I was like, I didn't think it would be, you know, as quick as it as it went. So from the time I felt the first contraction around six till the time she was born, it was 10 o'clock. So only four hours. We didn't even get to the hospital until after eight because my husband came here, picked me up and then we drove straight to the hospital. We were there after eight, like 8:15 maybe. And so I was only in the delivery room for maybe an hour and a half.
Lisa: 29:25
That's the way to go.
Melissa: 29:27
Yeah, it was pretty great. But at the same time you feel like you're in that vortex of time. Like it's just like, it was only an hour and a half, but it could have been two days.
Melissa: 29:40
That's just how strong the pain is, that you're like, "Oh like just get through each one, each one, each one," and I didn't have, I did have an IV, or a hep lock, in, but they didn't really use it. They were going to give me some antibiotics because I tested positive for the...
Lisa: 29:57
GBS.
Melissa: 29:59
I tested positive for that. So they tried get me the antibiotics into my system before she was born, but they didn't have enough time. It was so fast. So I was able to move around a lot easier than with the first one. And I actually gave birth, not laying on my back. Like I was hunched over, like not like yoga ball but like a yoga ball. It's more like an egg shape, I guess.
Melissa: 30:23
Peanut ball.
Melissa: 30:24
Yeah, the peanut one. And so like I was literally hunched over that, with my, like, face into the hospital bed on my knees and you know, she came. So you know, all I remember is the midwife saying, "You can look down, you can look down, she's coming, she's coming." And I was like, "I can't, I can't, I can't." It was such intense pain. Like my eyes were, like, closed and like I was squeezing my husband's hands, so like intensely, I just, I was like, "I can't even open my eyes right now. Like it's just so intense." But then when she was out, you know, obviously I was like, "Oh!" It just releases, and then, you know, then I was able to look down and see her and she was basically underneath me and it was, it was crazy. It was just like such a crazy experience and so different from the first one with the experience of having done it once. That was definitely helpful.
But then also just having the midwife, she was literally waiting for us outside. Like my husband pulled up in the car and she was standing outside waiting for us to come, which I was like, "That's crazy," because like the OB-GYN didn't even show up until like what felt like five minutes before Segovia was born. And so she was there the whole time, but yet she still tried to like give us a little bit of space where it was just us. So she could tell like when it was going to happen. And so she was like, "I'm just going to step out of the room, you know, do these next like couple of contractions. I'll be right outside, if you, like need anything, just, you know, Brian can come get me." And she was just standing out there listening to make sure that like, you know, she was there and ready for when it was time to push and she kept coming back in and she's like, "Let's try this position" and "Let's do this. It was almost like having a doula and a midwife all in one.
And so, and the nurses at that hospital seemed to love her. Like they really, like I even asked a few of them afterwards. I was like, "Oh, so what's the difference between like having Melanie and having like a typical OB-GYN?" And they're like, "It's just like night and day," you know, like they were just, they seemed to really love having that experience and, and that hospital also seems to be a little bit more natural-birth-friendly than Manhassett, so that I really enjoyed. Yeah, it was just a different experience altogether. I mean, I'm thankful it's over. But it's also incredible. Like it's hard. It's like one of the hardest things I'll ever...the hardest thing probably I'll ever do.
Lisa: 33:09
But like then you discovered those superpowers.
Melissa: 33:12
Exactly. But I'm glad that I did it, to know that like, oh, you know, millions and millions and millions of women, you know, have done this, you know, for centuries. And I'm glad that I was able to experience, like, what other women have done basically to keep us afloat, keep the world populated. It was much better I guess than I anticipated. Even though it was extremely difficult.
Lisa: 33:43
You were comparing the midwife to the OB in labor. Did you see differences in the care you received between the two care providers prenatally?
Melissa: 33:51
A little bit. I wouldn't say too much. She wasn't like very pushy about anything. Like, you know, like with the testing and all of that and like she was definitely more open about like, "Oh, you don't really have to have this test if you don't want to have it." Like, you know, it just, I don't even remember what it was, but like all the things, like when I went to the OB-GYN she was like, you know, "You have to have this and you have to do this and this and this and this." And it wasn't like that with Melanie, it was more like she was more like, "Yeah, well this one, like, they require us to do, but these, like, it's up to you. If you want to have the genetic testing, you can have it. If you don't want to have it, you don't have to have it." And I always thought like over 35 that you have to have that test, like to see if the baby's got down's syndrome, or you know any of that, and that's actually not true. Like I could have opted out of that. I chose to do it on my own account. Because, what's one more blood test? And I actually work with kids with special needs. So I was just curious if that is coming my way. But yeah, I really thought was something that was just required, you know, by like the state, or I don't know, law or something. And it's not. Like it's something they tell you it is, but it's not actually.
Lisa: 35:04
That is such a great observation. I hadn't heard it phrased that way before, but it really resonates that with a lot of OBs things both prenatally and in labor can come across as mandates versus when we get either a more flexible OB or really get good midwifery care, that we often feel like we have options in the way things are communicated. So thanks for sharing that.
Melissa: 35:25
Yeah, no problem. And, and I don't know, she just was also just much more positive I guess about the natural state of being. She's like, "Whatever you want." And you know, obviously I had concerns about the cholestasis early on before it ever would have happened. But you know, I was like, "If I do wind up getting it and I have to be induced, do I have to get Pitocin right away?" You know, because that's what the OB-GYN said. And she's like, "No," she's like, "there's so many other things we can do first." She's like, "I wouldn't wish that on you." She's like, "No, we can do all sorts of different things prior to having to resort to that if necessary."
So, you know, that was very reassuring in the beginning, and like part of the reason I chose like, "All right, I'm going down this path." You know, part of the reason I chose it to begin with, it just, it was just a very nice experience. I don't know, I would recommend it. I liked the aspect for me that like she's a midwife who practices mostly in the hospital because my husband wasn't really comfortable with like a home birth and as much as I would've considered it, I'm also a little, I don't want to say OCD, but I'm very type A. So having to plan that out and have all of that set up and ready to go was a little overwhelming to me. So I liked that she did mostly in a hospital. You know, if something were to have happened, she would have come to my house, you know, if the baby would have come before she was ready. But I liked that aspect for myself. But I"m definitely glad I went with a midwife either way, like on the second round. You know, I kind of wish I would have done it on the first round, but you know, at the time I just didn't really like have clear idea of who do you use, where to go, you know, like...
Lisa: 37:09
Yeah, why would you? So many of us don't have any clue about how great the midwifery model of care is until it's pretty late in our first pregnancy if not later. I often feel that when I teach about the midwifery model of caring class, it's teaching more to a second birth than a first, since most of the time folks are coming to class pretty late in pregnancy when it's harder to switch care providers.
Melissa: 37:29
Yeah, I would definitely recommend that for future birthing moms or pregnant moms or even when you are considering getting pregnant. Actually that's probably even a, a better time to find out is if you know before you're pregnant. Because once you are, you're just kind of, it's like a roller coaster of like, "Okay, here we go." You know, you can't get off the ride once it's actually there. So I'm, I'm really happy with that decision for the second one. I would recommend sending friends to Melanie if you know, if they want to go there, or other women who are interested in using a midwife but also want to use the hospital route. Like I would definitely like recommend going to her or somebody like her.
Lisa: 38:11
Do you want to share anything about your postpartum journeys?
Melissa: 38:13
The first round, I definitely remember it being a longer recovery. I was thankful to some friends who sent me like, a donut to sit on, because I didn't know you needed one of those. And I, because I had stitches first and I tore a little bit, the recovery was a little bit longer. I remember like thinking like, "Wow, I didn't realize that you were going to bleed for this long" or that, that your hormones are just "woooo!" the first like month or so. Like it's like up and down and up and down. I remember crying a lot, but like both for happy and sad reasons. I expected it with this one. So that was a little bit different. So I was actually like, "Oh, I know why this is happening." But the first one is like, "Wooo!" Whirlwind.
Another difference I think between the first one and Adelina is that although I didn't tear with her, so the recovery process seems to have gone a lot easier for me, that the cramping during like breastfeeding was a lot more with the second one than with the first. I also struggled a lot with breastfeeding with my first daughter and this one I'm seeming to do a lot better. I just didn't use a lactation consultant other than the ones in the hospital on either birth. I wish I had on the first, and I planned to with her, but things have been going well out. And then also just with the help of other friends who have gone through the process and just being a little bit more relaxed about it I think also helps.
But that's actually, I would say the hardest part honestly. Like the pregnancy is hard, but breastfeeding is, it's challenging. Like it is not for everybody, not easy going, especially in the beginning. It's just all consuming. Like I feel like all she does is eat, eat, eat, eat. Like I'm glad to be able to sit here for an hour and talk to you because only because she's wrapped up next to me asleep, but as soon as we're done and I take her out, we're going to have to go back to, to feeding again. And so yeah that is just...that I would say is the harder part. I think that there needs to be a lot more talk about it. I mean I think it's getting better. I think that like definitely even in hospitals, like they, they have people come in and talk to you and they offer, you know like little seminars and what not. But I think the harder part is when you're home, and so I think there just needs to be more availability, especially for, I want to say like lower income because a lot of them you have to pay out of pocket. And finding one that your insurance does take is like nearly impossible. I actually found one and then she wasn't available. And so that's why I didn't get them to come this time around. She told me, she'd go, 'I'll be available, you know, during those weeks.' And then when I finally contacted her then she's like, "Oh, I've had a family emergency, I can't come."
Melissa: 41:10
And I was like, "I just don't have the energy to like do all this crazy research to find another one that takes my insurance," so I just was like, "Let me just try and get through this and do my best to see if it works out for me." And I'm also just more relaxed that like if it doesn't, then I know what worked with my first daughter and we did wind up supplementing with her a lot and she's turned out just fine. So there were moments of, you know, doubt and whether or not like I was capable and you know, all of those kinds of feelings that come with it. But on this round I definitely...within the postpartum I'm more confident, I guess, and more comfortable with like, "Oh, okay, like, it is OK if like she needs like one bottle of formula tonight so that I can, you know, take a nap." I'm not like beating myself up about it as much as I did the first time around. So, yeah. So that's been good and a nice change from, you know, the first round of like uncertainty to, to now being like, "All right, I know we're going to get through this, you know, we'll just have to push through and keep feeding and, here we go." So yeah. Yeah.
Lisa: 42:32
Do you have any final parenting tips, especially for anyone who might have more than one at some point?
Melissa: 42:37
I have found that like giving a first child some one-on-one attention has not only been helpful for her, but also it's been helpful for me too because right before the second one is born, I was a little anxious about like missing out on that one-on-one time with my first daughter and, and also worried that this one would never get to experience that, you know, because she's the second one and she'll always have her sister, you know, so trying to balance time together, but also time one-on-one with my first daughter, one-on-one with the baby, and then also just my own time and time with my husband. Like that, that's very challenging. And I think six weeks in we're still figuring it out. I know that it's important to kind of address all of those parts and aspects of our life. So we continue to try. And I've taken Segovia out, you know, once or twice just me and her, since the baby's been born and I've left the baby with my husband, and it's been good. So I think we're going about it correctly...or not correctly. That's the wrong word, but in a way that works for us.
Lisa: 43:56
I know what you mean. In a healthy way. A healthy approach.
Melissa: 43:56
We're trying. We're trying. But I know there's definitely moments where, you know, like I get frustrated at my almost three year old and you know, I definitely have to step away or you know, take a break even if it's in the bathroom. She has a lot of needs that, you know, and some of them aren't being met, you know, just for the pure sake that there's a baby. And so I have to keep telling myself that's okay. You know, she's gonna, she's gonna be fine.
And one thing I have to say that, I mean that this isn't for every mom of two, but having her still go to her daycare that she goes to during the day is like a godsend. It's having time with the baby by myself and then also like her getting that socialization time, and the structure. I'm just thankful that we decided not to like keep her home because now I feel like this one, Adelina, is getting more of that mom time than she would have been able to do, had Segovia been here everyday like nipping at my feet, wanting to do all of her three year old things. So at least we get some hours during the day just us. And, and that, I would say, is definitely some words of advice is: even if you don't send them to like full time daycare, like maybe a day or two a week or a babysitter, or you know, something so that you have some bonding time with the next child or even...I can't imagine with a third or fourth. But yeah, with the second, like having that time is important. So that was about it, I guess.
Lisa: 45:39
That's great. I think there's so much wisdom in that, making it a priority to get alone time with each person in your family. So thank you for sharing that. Well, thank you so much for taking the time to chat. This has been wonderful and congratulations again on your second daughter's birth.
Melissa: 45:54
Thank you very much and yeah, thank you for all of your wisdom and help. It definitely was great. Thank you.
Lisa: 46:04
So that’s Melissa’s 2 birth stories. I’ll comment briefly on 4 things Melissa mentioned: cholestasis, the labor drink “switchel”, switching care providers, and a mental strategy of minigoals as a golden one for labor. In case you want to learn more about cholestasis, I’ve linked to information about the condition in the show notes for Episode 15 at birthmattersshow.com. Cholestasis affects only around 1 to 2 in 1000 pregnant women in the United States (or less than 1%), but it’s more common in Latina women. In the Latina population, about 5% develop the condition.
The labor drink Melissa mentioned loving, called “switchel”, is known as nature’s Gatorade or a great labor-ade, so to speak. It’s super simple to make and is made of simple ingredients -- ginger, apple cider vinegar, maple syrup, and water. I’ll paste the recipe for it in this episode’s show notes, again at birthmattersshow.com Also, I wanted to mention that it’s almost never too late to switch care providers if you start to feel like you aren’t aligned with one who is a good fit for you and the kind of birth you’d like to have. I can’t speak for all locations, but I know this is true here in NYC. The options do significantly diminish in the 3rd trimester, but there are options. This is something your childbirth educator or doula can help provide some referrals and guidance on.
Finally, I wanted to emphasize how great a strategy Melissa mentioned and used can be for labor. A lot of people call labor a "marathon of indeterminate length.” While this might not sound like a very encouraging thing, I think it’s really important to think of it this way strategically. The encouraging thing is that your body has the innate ability to do this hard work of giving birth without vigorous training. The kind of training that is most helpful is more gentle bodywork, and mostly mindset preparation. Anyway, along the strategic lines, Melissa mentioned, “I can do anything for 60 seconds.” One thing I recommend is for labor support to keep the mini-goals strategy in their back pocket. Many of us hit a wall -- one that’s psychological but then, due to the huge mind-body connection, can feel very physical -- at some point in what tends to be a long first labor. If that happens, it’s incredibly helpful to have our labor support break it down for us. Encourage her by saying something like, “Let’s just get through the next 5 contractions.” Don’t start at 1, because you need room for negotiation. If you just say one, there’s nowhere to go from there if she feels like that’s too much! Many people use this kind of strategy in a challenging workout or in an endurance athletic event, and this strategic tool can be all the more useful when no one knows how long you have to do this and where the finish line is.
Okay, here’s a little bit of what we have for you next week!
Speaker 4:48:56
Have you seen the show "Stranger Things"?
Lisa: 48:59
Yes. Yup.
Speaker 4:49:00
Okay, so in this show there's the Upside Down. It's like this alternate universe. And when I was, now I know I was in the transition phase, I kept saying "I'm in the Upside Down!"
Lisa: 49:16
Totally.
Speaker 4: 49:17
It felt like I was losing consciousness!
Lisa: 49:20
One phrase I’ll leave with you. When you’re in labor, at times if you’re struggling, just tell yourself: “I can do anything for 60 seconds!” See ya next week and be well!---END---