My due date was on April 14, 2017, but the day came and went uneventfully. On 40 [weeks] 4 [days pregnant], my midwife agreed to strip my membranes. I was 2.5 cm dilated, but still no labor. Throughout the week, my Mom and I did a lot of walking to keep busy. On 40+6, at approximately 5 p.m., I began to feel belly tightness and began keeping an eye on the time, although I wasn’t sure that they were contractions. At that point, they were about 15 minutes apart, lasting about 15-20 seconds at a time. As we walked home the mile from the stores, the pattern continued, leaving us saying, “Well, this could be the beginning…” When Tim was home, too, we continued to feel fairly skeptical that it was actually the start of labor, since I was able to comfortably talk and do other activities while contractions were happening.
We went to bed around 10:30 p.m., and by 11, I began to feel more uncomfortable and had a hard time getting settled. I was using deep breathing and tried to get into comfortable positions out of bed. I soon woke Tim and asked him to begin timing and helping me through contractions. At that point, they were already under 5 minutes apart, but lasted no longer than 30 seconds. At 1 a.m., we called our practice to let them know that labor was in progress. The OB called Tim back and said that we could come into the hospital at any point but that, unfortunately, the birth center we were planning to go to was full of laboring women and we would need to go to regular labor and delivery. We were disappointed to hear it, certainly, but I also was able to mentally let go of that part of our birth plan. At this point, with labor in full swing, I knew that my top priority was having the baby safely and the setting mattered much less.
By about 3:00 a.m., I decided that I wanted us to go to the hospital because I did not want to be in too much more intense labor while we were in transit. The car service arrived and we drove through the early morning streets of Queens and Manhattan.
Once at the hospital, around 4:30 a.m., we went to Labor and Delivery triage. We quickly learned from the staff that it wasn’t just the birth center that was full--L&D was at capacity and at present no rooms were available. Eventually, they brought me to a room to be assessed and I was 7 cm dilated. I was therefore in active labor and would be given a room in L&D…once one opened up. I continued to labor standing or sitting, with Tim’s continued support.
At 5:30 a.m., we were sent to an L&D room, and the OB arrived. She said to make sure to let her know once there was pressure, and that she planned to stay on duty for a few more hours to deliver me and another laboring patient. Mom and Tim continued to be great supports. Tim would breathe with me and massage my back. Mom would take over when Tim needed a break.
At 9:30 a.m., the OB came back to examine me. She pronounced me 6-7cm dilated. I felt really discouraged although I tried not to dwell on it. All those hours and no more dilation at all? I continued laboring, but was certainly getting more tired.
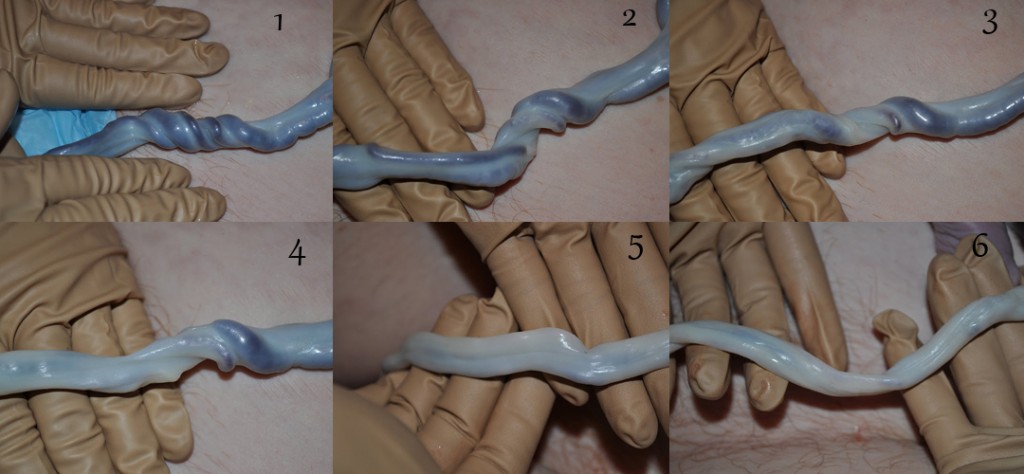
My midwife arrived, taking over for my OB, and stated that it was time this baby came out. She suggested that we artificially rupture the membranes. We agreed, hoping to speed baby’s arrival. There was slight meconium staining. I was also starting to feel a lot of lower-back pressure, so my midwife guessed that the baby might be posterior, which could also account for the slow labor. She also wondered whether the baby could be wrapped in the umbilical cord, slowing her descent. Thankfully, though, the baby’s heart rate remained strong whenever monitored. She said we would wait and see. I was around 8.5 cm dilated.
I felt quite exhausted, having been in labor all night, and was starting to be worried that I wouldn’t have energy for pushing once the time came. I asked for nitrous oxide to be made available to me. I really appreciated the nitrous oxide--although I could still feel the contractions, I cared about them a little less. I felt like I was being wrung out. Throughout, Tim and Mom continued with me, reminding me to breathe, telling me I could do it, and telling me that I was doing a good job. I didn’t feel like I was--I felt like I might not make it, and was scared that I couldn’t bring the baby into the world. I alternated between feeling really hot, and shivering uncontrollably. I kept using the nitrous oxide but it was losing its ability to take much of the edge off the intensity while I was in transition.
The midwife explained that it might be necessary to use vacuum extraction and that if the baby didn’t come within three tries, then the next step was the OR. I understood. Certainly, I didn’t want either of those outcomes, but if they were necessary to bring this baby safely, I was okay with it. She checked me one more time and I was finally fully dilated at around 5 p.m. At that point, I really wanted to push, but she asked me to hold off a few minutes while everything was prepared.
My midwife had Mom and Tim each help me hold up one leg while I would push during the contractions. The baby started at -1 station. By the point that I was given the go-ahead to push, I felt a return of energy. This felt good. I could handle this part. Sure, it still really hurt (no nitrous oxide now) and was very hard work, but it was much, much better than just tolerating the contractions coming in waves. The OB came in--she was clearly asked to be on call in case we’d needed to escalate to further interventions. She and the midwife agreed that I was pushing well and productively, so she left.
Coached by my midwife, and encouraged by Tim and Mom, I kept pushing. They were excited that they could see the head. The midwife asked if I wanted to feel it, and I said no--if we could see the head, then we were close, and I just wanted to keep going! She again asked me to wait and all the final preparations were put in place. She stated that she would need to make a cut to assist the birth; although we had hoped to avoid an episiotomy, our top priority was a safe birth, and we said okay. With one final set of pushes, the baby came sliding into the world in an incredible sensation. Instant relief! Baby began to cry loudly. The midwife quickly clamped the cord, (we’d planned with her for delayed cord clamping, but I think the worry about the possibility of the cord around the neck, and the meconium may have changed that option). She announced that the umbilical cord was not around the baby, and promptly handed her to the pediatrician. He quickly suctioned baby’s nose and mouth as she continued to wail heartily, with limbs flailing in all directions. Tim’s face and Mom’s were so excited--there was a joyous, even euphoric, atmosphere in the room.
As soon as baby was born, I felt incredible, and all I wanted was to have her on me. Madeleine. My baby. She seemed so long, so big, and I marveled that she could have fit inside me. I could see her being tended in the corner and asked that she be brought to me as soon as possible. After what felt like a long time, but was probably less than 5 minutes, there she was on my chest. I talked to her, called her by name, and she stopped crying and seemed to be listening to my voice. I told her how proud I was of her, proud of how hard she had worked to come into the world. It felt surreal that this was my daughter, this lively little being blinking in the new world.
While the midwife stitched me up, (I tore in addition to the episiotomy), and delivered the placenta, I marveled at little Madeleine. She was working her lips, bobbing her head up and down, and using her hands as she searched for the breast. Her little feet were pushing against my belly as she propelled herself around in her quest. We guided her just a bit, and she was able to latch on independently. She went on to nurse for nearly 45 minutes, drinking her fill of colostrum. Born at 5:48 p.m. on April 21, she was 7 lbs 10 oz,, 20.5 inches long, and absolutely perfect.
I was overwhelmed with love for my little girl, and gratitude for the steadfast support of Tim and Mom. I knew I would not have made it without them. The end result--a safe, healthy arrival for little Madeleine--made it worth it, and I was intensely grateful.